How to Check for Prostate Cancer at Home
Home prostate cancer detection is becoming a mainstream approach. It’s akin to checking your car’s oil before a long drive: it’s quick, private, and wise. These at-home tools don’t diagnose cancer but alert those who need further medical evaluation.
Today, you can find finger-prick PSA kits that send blood to labs for analysis. There are also urine gene tests like MyProstateScore 2.0 (MPS2) that don’t require a digital rectal exam. Studies from Vanderbilt and the University of Michigan have backed urine testing without a DRE. Now, several U.S. vendors offer kits focused on clinical use.
The advantages are evident: more men in remote areas can access these tests, telehealth follow-ups are easier, and privacy is maintained. A prostate cancer self-test can detect PSA changes, urine gene signatures, or symptoms early. This can help avoid unnecessary biopsies and catch significant cancers sooner.
Understanding Prostate Cancer And The Role Of Home Screening
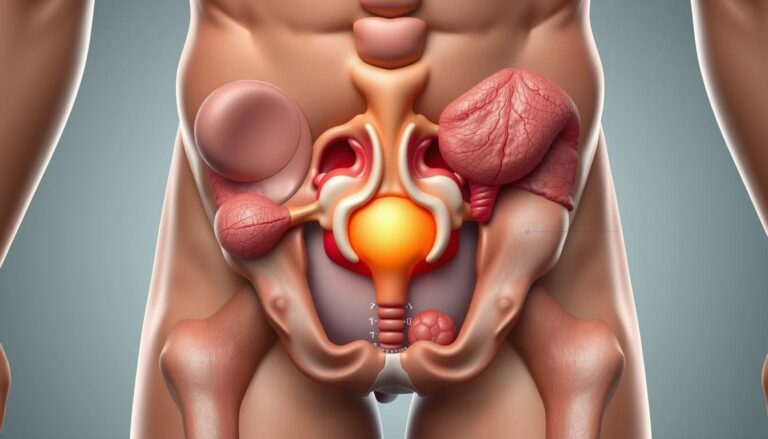
Prostate cancer occurs when cells in the prostate gland grow abnormally, forming a tumor. Many early cancers show no symptoms, making screening vital. Men experiencing urinary changes, blood in urine or semen, persistent pelvic pain, or new back pain should seek evaluation. These signs can indicate cancer or benign conditions like benign prostatic hyperplasia or prostatitis.
What Prostate Cancer Is And Typical Symptoms To Watch For
Prostate cancer is a malignant growth in the prostate gland that may grow slowly for years. Early stages often have no clear symptoms. Symptoms like a weak stream, trouble starting, frequent trips at night, or an urgent need to go are common. Blood in urine or semen and persistent pain in the pelvis or lower back may also occur.
Screening tools like PSA blood testing detect biochemical changes before symptoms appear. A digital rectal exam can find nodules that PSA misses. For those interested in a prostate cancer self-check or a prostate exam at home, remember to seek formal testing for any new symptoms.
Difference Between Screening And Diagnosis
Screening aims to identify possible problems before they become diseases. Common screening methods include PSA blood tests, digital rectal exams, and urine biomarkers. These tests suggest higher risk but cannot confirm cancer alone.
Diagnosis requires further tests. Clinicians often repeat PSA, order imaging like multiparametric MRI, and perform a biopsy to obtain tissue for histopathology. PSA levels are used as a guide without a single universal cutoff. Elevated values usually trigger more evaluation, not an immediate diagnosis.
Why At-Home Screening Can Increase Early Detection And Access In The United States
At-home screening lowers barriers for men in rural or underserved areas by adding privacy and convenience. Kits that collect finger-prick blood or urine and send samples to accredited labs support telehealth visits and faster triage. Reliable home options help men start a conversation with their clinician earlier.
Research from Vanderbilt and the University of Michigan shows promising results for urine-based tests that detect gene signatures linked to significant cancer. These assays can reduce unnecessary biopsies and extend safe screening to men who might skip clinic visits. Choosing a kit for a prostate exam at home requires clear instructions and lab accreditation.
| Aspect | Screening Purpose | Role In Access |
|---|---|---|
| PSA Blood Test | Detects biochemical changes before symptoms | Home kits allow early detection and prompt follow-up |
| Digital Rectal Exam (DRE) | Physical check for nodules or irregularities | Requires clinician, but results complement home screening |
| Urine Biomarkers | Detect gene signatures tied to high-risk tumors | At-home urine collection can reduce needless biopsies |
| Self-Check Awareness | Spotting symptoms that prompt testing | Encourages timely clinical visits after a prostate cancer self-check |
| Telehealth Integration | Connects test results with clinician guidance | Improves access in remote areas and supports follow-up |
How To Check For Prostate Cancer At Home
Home screening has opened new avenues for men to monitor their prostate health. The at-home prostate cancer screening, prostate cancer self-test, and DIY prostate cancer screening are all key in early detection. They also prompt timely clinical care.
Overview Of Methods Available For At-Home Screening: Urine, Blood, And Symptom Checks
Finger-prick blood kits measure total PSA and some include free PSA. Users collect a small sample, mail it to a certified lab, and receive numeric results with lab notes. These kits function like standard clinic tests but from home.
Urine-based assays analyze gene markers tied to aggressive disease. Tests such as MyProstateScore 2.0 use multiple markers to help flag higher-risk cases without a digital rectal exam. Urine options are growing as noninvasive alternatives.
Symptom tracking remains vital. Noticing new urinary changes, nocturia, weak stream, or pelvic discomfort can prompt a prostate cancer self-test or a clinician visit. Symptom checks do not diagnose cancer but guide next steps.
When At-Home Screening Is Appropriate And When To Seek A Clinician
At-home testing suits men 40 and older who want routine monitoring, those with a family history of prostate cancer, and Black African or Black Caribbean men at higher risk. People seeking peace of mind may choose a DIY prostate cancer screening service with accredited labs.
Immediate clinical attention is required for alarming signs: heavy bleeding, severe unexplained pelvic pain, acute urinary retention, or a very rapid rise in PSA. Elevated or unusual home results should trigger prompt follow-up with a primary care doctor or urologist.
How To Interpret At-Home Screening As Part Of A Broader Clinical Pathway
Put home results in context. Age, baseline PSA trends, the free-to-total PSA ratio, urine gene signatures, and current symptoms all affect interpretation. One elevated value rarely means immediate biopsy; trends matter more than a single number.
Common next steps after an abnormal home test include repeat PSA testing, prostate MRI, referral to a urologist, or biopsy when indicated. Reliable home services offer lab accreditation and clear referral pathways to help integrate results into clinical care.
| Method | What It Measures | Best Used For |
|---|---|---|
| Finger-Prick Blood PSA | Total PSA; some report free PSA for ratio analysis | Routine monitoring and initial screening at home |
| Urine Gene Assay (e.g., MPS2) | Multiple gene markers linked to high-grade cancer | Noninvasive triage to reduce unnecessary biopsies |
| Symptom Check | Self-reported urinary and pelvic signs | Triggers for testing or urgent clinical evaluation |
At-Home PSA Testing: What It Measures And How It Works
Home PSA testing offers a quick look at prostate health without needing a doctor’s office. It’s a practical option for those curious about prostate cancer screening at home. Or for those who prefer a private test before a clinic visit.
What PSA Is And Why Labs Measure Total And Free PSA
PSA stands for prostate-specific antigen, a protein from prostate cells released into the blood. Labs measure total PSA, the full amount, and free PSA, the unbound portion.
Doctors use the free-to-total PSA ratio to distinguish between benign conditions and cancer risk. A lower ratio may prompt further testing. Many services measure both and offer an interpretation to guide follow-up decisions.
How Home PSA Kits Collect Samples And Send Them To Accredited Labs
Home PSA kits use a small lancet for a finger-prick blood sample. They include tubes, instructions, and a prepaid mailer for lab analysis. Labs must meet standards like CLIA in the U.S. or ISO 15189 internationally.
Results are usually ready in a few days. Validated services provide support, explaining abnormal results and suggesting next steps.
Factors That Can Raise Or Lower PSA And How To Prepare For Testing
PSA levels can change for various reasons. Age and BPH commonly increase PSA. Infections and recent ejaculation can also raise levels.
To ensure accurate results, avoid ejaculation for 48 hours and skip intense cycling or prostate stimulation. Inform the lab about recent procedures or infections when registering the test.
A single high PSA doesn’t confirm cancer. It’s a signal for further evaluation, like a repeat test or MRI. For those considering a self-exam or home screening, a home PSA test is a useful tool.
Urine-Based Home Tests And New Noninvasive Options
Urine-based testing has revolutionized home prostate cancer detection. New noninvasive methods seek molecular signals, not just protein levels. These tests provide clearer risk information from a simple urine sample, making at-home screening more accessible.
Exploring how urine tests, like MyProstateScore 2.0, function and what they detect.
MyProstateScore 2.0 examines urine for an 18-gene signature linked to aggressive prostate cancer. It identifies molecular markers for significant tumors. This focus helps differentiate between high-risk and low-grade cases, guiding treatment decisions.
Validating urine tests without a DRE through Vanderbilt and University of Michigan research.
Researchers from Vanderbilt and the University of Michigan published findings in The Journal of Urology. They showed urine sampling without a digital rectal exam is highly accurate. This supports the use of at-home prostate cancer screening.
Potential to reduce unnecessary biopsies and support telehealth or remote screening.
MyProstateScore 2.0 could prevent 34%–53% of unnecessary biopsies by ruling out significant disease. This reduction minimizes procedure risks and patient anxiety. Noninvasive urine testing also enhances telehealth options for men in remote areas.
| Feature | What It Measures | Benefit For Patients |
|---|---|---|
| MyProstateScore 2.0 | 18-gene expression signature in urine | Targets clinically significant cancers; aids in deciding on biopsy |
| Non-DRE Collection | Voided urine without prostate massage | Enables true at-home testing and easier telehealth workflows |
| Biopsy Reduction | Negative molecular risk profile | Potential to prevent 34%–53% of unnecessary biopsies |
| Clinical Integration | Gene-level risk stratification plus PSA | Improves overall risk assessment and follow-up planning |
- Urine prostate test data complement PSA in risk decisions.
- MyProstateScore 2.0 offers molecular detail useful for clinicians and patients.
- At-home prostate cancer screening via urine enables wider access and easier monitoring.
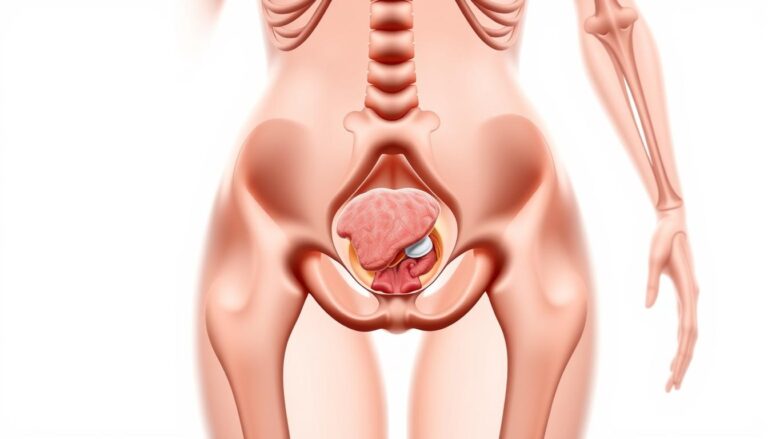
Self Prostate Exam And What Men Should Know About A Physical Self-Check
While a self prostate exam might seem straightforward, it’s not as simple as it appears. A true digital rectal exam (DRE) demands clinical training to accurately assess the prostate’s shape and texture. Trying to perform a prostate exam at home provides little diagnostic value and can lead to misinterpreting normal anatomy as a problem.
Limitations And Risks Of Attempting A Self Prostate Exam At Home
A clinician’s hands-on assessment can identify posterior lumps that a self-check would likely miss. Misinterpretation can result in either false reassurance or unnecessary alarm. Without proper technique or sterile conditions, probing the rectal area can cause discomfort or minor injury.
Dependence on a prostate cancer self-check done alone reduces sensitivity and specificity compared to professional exams and PSA testing. A clinician combines palpation, history, and lab results to form a clearer picture.
What Signs You Could Feel Or Notice That Warrant Professional Evaluation
Some changes are worth prompt evaluation. New, persistent lumps or firm nodules, though hard to detect at home, should prompt a clinician visit if suspected. Constant pelvic or rectal pain matters when it does not resolve.
Visible blood in urine or semen, sudden urinary obstruction, frequent nighttime urination that worsens, or notable changes in stream and urgency deserve attention. These symptoms can come from benign prostate enlargement or infection, yet they require assessment.
Skip DIY rectal exams. Use symptom awareness, validated home tests, and telehealth to gather information. This approach supports a focused visit with a urologist or primary care doctor when a prostate cancer self-check or home test suggests further evaluation.
DIY Prostate Cancer Screening Kits: Choosing A Reliable Provider
Choosing a home prostate cancer detection kit is like selecting a travel companion. It’s about trust, clarity, and a clear plan. A reliable provider offers lab-grade testing, easy-to-follow instructions, and a clear path to clinical care if needed. This guide will help you know what to look for before buying a DIY prostate cancer screening or prostate cancer self-test kit online.
Key Features To Seek
- Laboratory accreditation such as CLIA in the U.S., ISO 15189, or UKAS for overseas labs.
- Measurement of both total and free PSA with a clear ratio reported for context.
- Usability-tested kits and step-by-step sample collection instructions written in plain language.
- Reflex testing protocols, where elevated total PSA triggers free PSA or additional assays without extra hassle.
Privacy, Handling, And Follow-Up
- Discrete packaging and prepaid return mailers protect privacy during shipping.
- Secure electronic delivery of results with options for clinician or nurse callbacks for abnormal findings.
- Fast turnaround times — many reliable services report results within about five business days.
- Clear referral paths to urologists or health systems if further evaluation is required.
Red Flags To Avoid
- Products that claim an instant at-home definitive cancer diagnosis. Screening never confirms cancer on its own.
- Kits that omit free PSA, report only a single number, or fail to show laboratory accreditation.
- Anonymous sellers without published sensitivity and specificity data or clinical validation studies.
- Poor or missing sample-handling instructions, no secure result delivery, and no clinical follow-up option.
When selecting a provider for a prostate cancer self-test or DIY prostate cancer screening, aim for safety and simplicity. Seek transparent lab practices, clear communication, and a pathway to clinicians for results needing attention. With the right kit, home prostate cancer detection can be a valuable first step in your care journey.
Preparing For At-Home Tests And How To Collect Valid Samples
Before collecting a sample, a few simple steps are essential. Proper preparation ensures accurate results when checking for prostate cancer at home. It also supports reliable home prostate cancer detection.
Start with a short checklist before testing. Avoid ejaculation for 48 hours to prevent PSA spikes. Skip testing after a prostate biopsy, catheterization, or digital rectal exam. Also, wait after prolonged cycling or an active urinary infection. Inform the kit provider about any hemorrhoids or anal fissures for guidance on comfort and technique.
Follow the kit’s finger-prick blood instructions carefully. Use the lancet provided and wipe the first drop away if instructed. Collect the required drops into the provided card, tube, or microcontainer and seal it exactly as shown. Place samples in the provided biosecure bag with the absorbent pad. Use the prepaid mailer and label the package as instructed for safe return.
Urine kits vary by design. Some require first-catch urine, while others ask for a sample after a short prostate massage. Validated urine tests such as MyProstateScore 2.0 work without a DRE, making them convenient for a prostate cancer self-test at home. Time the collection as the instructions specify and avoid contaminating the cup rim.
Pack samples into the discreet mailer supplied. Ensure all forms are filled out, the barcode is visible, and the return label is secure. Drop the package at the designated courier point the same day when possible to preserve sample integrity.
After mailing, accredited labs run the analysis. Typical turnaround ranges from a few days to about five business days, depending on the provider. Many services offer secure online delivery of results and a follow-up call with a nurse or clinician when findings require explanation.
Keep receipts and tracking numbers until results arrive. Clear communication from the lab reduces worry and helps plan the next steps if abnormal numbers appear. A stepwise approach that ties home testing into clinical care improves the value of a prostate cancer self-test and strengthens overall home prostate cancer detection.
| Step | Why It Matters | Practical Tip |
|---|---|---|
| Abstain From Ejaculation 48 Hours | Prevents transient PSA elevation that can skew results | Plan around intimate activity and note dates on the kit form |
| Avoid Recent Prostate Procedures | Recent biopsy, catheter use, or DRE can alter markers | Wait 4–6 weeks after procedures; consult the provider if unsure |
| Follow Finger-Prick Collection Steps | Ensures sufficient volume and reduces contamination | Warm the hand, wipe first drop if asked, collect slowly |
| Observe Urine Timing | Some tests need first-catch urine; others ask for post-massage | Read instructions, label sample time, and avoid rinsing beforehand |
| Use Provided Biosecure Packaging | Protects sample during transit and meets lab standards | Include absorbent pad, seal bag, and use prepaid mailer |
| Expect Lab Turnaround | Timely analysis and secure result delivery reduce anxiety | Track shipment and check provider timelines (often ~5 business days) |
| Request Clinical Follow-Up | Abnormal results need interpretation and next-step planning | Choose providers with nurse or clinician callbacks |
Interpreting Results And Next Steps After An Abnormal Home Test
A home screen that flags a concern begins a clinical conversation, not a diagnosis. A raised value on a prostate cancer self-test or an unexpected urine biomarker suggests the need for follow-up. Causes range from benign prostatic hyperplasia and prostatitis to recent ejaculation or procedures. Clinicians place any abnormal result into that context before deciding what comes next.
Understanding That Screening Tests Do Not Confirm Cancer
Screening catches signals. It does not confirm disease. A single elevated PSA from an at-home prostate cancer screening can reflect temporary inflammation or lab variation. Many doctors repeat testing to confirm a trend before ordering invasive steps.
Common Next Steps After An Abnormal Home Test
- Repeat PSA or repeat the at-home kit to check for persistent elevation and reduce false positives.
- Order bloodwork or urine tests to rule out infection and review clinical history.
- Refer to a urologist for focused evaluation when levels stay high or symptoms persist.
- Consider a multiparametric prostate MRI to localize suspicious areas and guide decisions.
- If imaging or risk calculators warrant, perform a targeted or systematic biopsy for histologic diagnosis.
How Clinicians Use Ratios And Urine Gene Tests To Reduce Unnecessary Biopsies
Physicians use total and free PSA ratios to sharpen risk estimates. A low free-to-total PSA ratio raises concern for cancer. Many labs automatically reflex to free PSA when total PSA sits in an intermediate range.
Urine gene assays, such as assays modeled on MyProstateScore 2.0, help rule out clinically significant tumors. In study groups these tests avoided a substantial share of unnecessary biopsies. Combining PSA metrics, urine biomarkers, MRI findings, and personal risk leads to more precise decisions and fewer needless procedures.
Clear communication matters at every step. When an at-home prostate cancer screening flags an issue, timely discussion with a primary care clinician or urologist helps map the safest, least invasive path forward.
Who Should Consider At-Home Prostate Cancer Screening And Risk Factors
At-home tests offer a practical entry point for men interested in prostate health. They act as a starting point for those pondering prostate screening and those who prefer a gentle introduction before clinic visits.
Age Guidelines And High-Risk Groups
Screening discussions often begin at 40 for men with higher risk profiles. A family history, such as a father or brother diagnosed before 60, heightens urgency. Men of Black African or Black Caribbean ancestry face a higher risk and may be advised to start screening earlier.
U.S. healthcare providers adjust screening timing and frequency based on individual factors. These include life expectancy, past health, and patient preferences, guiding decisions on when and if to test.
Balancing Benefits And Harms
Screening can identify cancers early, when they are more treatable. Yet, it also detects slow-growing tumors that may never cause harm. This can lead to overdiagnosis and overtreatment, with its own set of side effects.
Using tests like free-to-total PSA ratios, urine gene panels, or MRI can help avoid unnecessary biopsies. These tools focus care on what’s truly necessary, reducing unnecessary interventions.
Incorporating Personal Risk, Symptoms, And Shared Decision-Making
Home testing is most effective as part of a broader strategy. A prostate cancer self-check or home PSA kit can spark a conversation with a healthcare provider. Abnormal results should prompt a clinician-led evaluation, not immediate panic.
Decisions are based on personal risk factors, current symptoms, and individual values. Open discussions with a urologist or primary care doctor help strike a balance between vigilance and the risks of overtesting.
Practical questions—such as how to check for prostate cancer at home, which kit to use, and when to see a specialist—are best addressed with a trusted healthcare provider. This collaborative approach ensures screening remains relevant and aligned with personal priorities.
Conclusion
At-home screening is a practical first step for men seeking privacy and easier access. Home PSA tests and urine gene panels provide valuable insights into risk levels. They serve as a compass, guiding the decision to seek specialist advice next.
Key takeaways include following preparation tips like 48-hour sexual abstinence and avoiding recent prostate procedures. Choose accredited providers that report total and free PSA when relevant. Expect lab-based analysis with clear follow-up. A prostate cancer self-check via validated kits can flag issues early while protecting privacy.
Recent research from Vanderbilt and the University of Michigan suggests urine tests such as MPS2 can rule out clinically significant cancers without a DRE. This may cut unnecessary biopsies. Such progress strengthens home prostate cancer detection as a viable option for telehealth and remote screening programs.
Men in higher-risk groups or those with symptoms should view at-home results as the start of a conversation, not a conclusion. Use validated home tests to inform shared decision-making with a clinician. This guides timely next steps when needed.
FAQ
What Is Prostate Cancer and what symptoms should prompt concern?
Prostate cancer is a malignant growth in the prostate gland. Many early cancers cause no symptoms. Signs that should prompt clinical evaluation include new or worsening urinary changes (slow stream, hesitancy, frequency, getting up at night), blood in urine or semen, persistent pelvic or back pain, or sudden and severe urinary obstruction. These symptoms often overlap with benign conditions such as benign prostatic hyperplasia (BPH) or prostatitis, so clinical assessment is required to determine the cause.
Can at-home screening tests diagnose prostate cancer?
No. At-home tools—finger-prick PSA kits and urine gene assays—are screening methods that flag elevated risk. They can identify who needs further workup but do not confirm cancer. Diagnosis requires follow-up testing such as repeat PSA measures, prostate MRI and tissue biopsy for histopathologic confirmation.
What at-home screening options are currently validated?
Validated home options include finger-prick blood kits that measure total and sometimes free PSA and send samples to accredited labs, and urine-based gene assays such as MyProstateScore 2.0 (MPS2). Recent studies from Vanderbilt and the University of Michigan support urine testing without a DRE, making at-home urine collection a growing, noninvasive option.
How do PSA and free-to-total PSA ratio help clinicians?
PSA is a protein produced by the prostate and measured in blood. Total PSA is the overall level; free PSA is the unbound portion. The free-to-total PSA ratio helps distinguish benign enlargement from higher cancer risk—lower ratios can suggest greater likelihood of significant cancer. Lab-measured ratios complement other tools to guide need for imaging or biopsy.
How do home finger-prick PSA kits work and are they reliable?
Home kits use lancets to collect capillary blood drops into a supplied device or card. The sample is sealed, mailed in a prepaid discreet package to a certified lab (CLIA, UKAS/ISO 15189 or equivalent), and analyzed. Clinically validated services provide usability testing, measure total and free PSA when indicated, and return results with interpretation and follow-up pathways.
How do urine tests like MyProstateScore 2.0 work and what do they detect?
MPS2 analyzes multiple gene markers in urine that are associated with high‑grade prostate cancer. The assay targets molecular signatures tied to clinically significant disease and helps stratify risk beyond PSA alone. Because validated versions can be collected without a DRE, they support convenient home sampling and remote assessment.
When is at-home screening appropriate and when should someone see a clinician urgently?
At-home screening is suitable for men 40+, those with a family history, Black African or Black Caribbean men at higher risk, and men who want monitoring or a private first step. Seek urgent clinical care for alarming symptoms such as heavy bleeding, severe unexplained pelvic or back pain, acute urinary retention, or rapidly rising PSA—these require prompt in-person evaluation.
Is attempting a self prostate exam at home advisable?
No. A true digital rectal exam (DRE) should be performed by a trained clinician. Self-exam is unreliable, can cause injury, and may give false reassurance or unnecessary alarm. Rely on symptom awareness and validated at-home tests instead of attempting a self DRE.
What factors can temporarily raise or lower PSA and how should one prepare for testing?
PSA can be affected by age, BPH, prostatitis or urinary infections, recent ejaculation, prostate stimulation (including DRE), prolonged cycling, or recent prostate procedures (biopsy, catheterization). To reduce transient rises, abstain from ejaculation for 48 hours before testing, avoid recent prostate procedures or heavy cycling, and postpone testing if there is an active urinary infection.
How should finger‑prick blood and urine samples be collected and mailed?
Follow the kit instructions closely. For finger‑prick blood, use the provided lancet and collect required drops into the supplied device or card, seal as directed, and place in the biosecure container with absorbent padding. For urine tests, follow timing guidance (some assays specify first-catch urine; MPS2 can be collected without DRE). Use the prepaid discreet mailer and courier/post drop specified by the provider.
What happens after mailing a home test sample and how quickly are results returned?
Accredited labs analyze samples; turnaround varies by provider but often occurs within several working days (some services advertise about five working days from receipt). Quality providers deliver secure results and offer nurse or clinician follow-up for abnormal findings, with clear signposting to local care or urology referral.
If a home test is abnormal, what are the common next steps?
Follow-up typically includes repeating PSA to confirm trends, considering multiparametric prostate MRI to localize suspicious areas, and referral to a urologist. If imaging or clinical risk suggests, a targeted or systematic biopsy may be recommended for histologic diagnosis. Clinicians integrate PSA trends, free-to-total ratios, urine gene test results, MRI findings and patient factors in decision-making.
How can urine gene tests reduce unnecessary biopsies?
Urine assays like MPS2 are designed to rule out clinically significant cancers. Vanderbilt and University of Michigan data indicate such tests could have avoided roughly 34%–53% of unnecessary biopsies in study cohorts by identifying men at low risk for high-grade disease, allowing safe avoidance of invasive procedures when combined with clinical judgment.
What should men look for when choosing a DIY prostate cancer screening kit online?
Choose providers with laboratory accreditation (CLIA, ISO 15189, UKAS), transparent clinical validation, and kits that measure total and free PSA when relevant. Look for clear step-by-step instructions, secure result delivery, discreet packaging, reasonable turnaround time, and a defined clinical follow-up pathway (nurse or clinician contact and referral options). Avoid tests that promise instant diagnoses, lack free PSA measurement, or do not disclose lab accreditation and sensitivity/specificity data.
Who should consider at-home prostate cancer screening and how do risk factors change timing?
Men aged 40 and older who wish to monitor prostate health, those with first-degree family history of prostate cancer diagnosed at a younger age, and men of Black African or Black Caribbean ancestry should consider earlier or more proactive screening. Clinicians tailor timing and tools to individual risk, life expectancy and preferences.
How should home screening results be used in shared decision-making with a clinician?
Treat home results as a compass pointing toward whether to seek further evaluation. Discuss the results with a clinician who will weigh age, baseline PSA trends, free-to-total PSA ratio, urine biomarker findings, symptoms and personal risk. Together, patient and clinician decide on next steps—repeat testing, MRI, biopsy or continued monitoring—to balance early detection against risks of overdiagnosis and overtreatment.