Radiation for Prostate Cancer: Possible Side Effects
Radiation therapy for prostate cancer employs focused energy, such as X-rays, protons, or radiopharmaceuticals, to damage cancer cells’ DNA. This approach aims to slow or halt tumor growth. Machines like linear accelerators and proton centers are used to shape beams. Brachytherapy, on the other hand, involves placing radioactive seeds directly inside the prostate.
Various methods, including IMRT, VMAT, SBRT, MRI‑linac, and systemic agents like lutetium Lu 177 vipivotide tetraxetan, alter how the dose is delivered. This affects which tissues are exposed to radiation.
The objectives of treatment vary, from curing localized disease to shrinking tumors post-surgery or alleviating bone pain in advanced stages. External beam therapy typically requires daily outpatient sessions lasting several weeks. In contrast, hypofractionated and stereotactic schedules are shorter. Brachytherapy involves short anesthesia and a brief hospital stay. Radiopharmaceuticals are administered via infusion on set schedules.
Like all cancer treatments, radiation therapy side effects include both immediate and delayed reactions. Many patients experience temporary urinary or bowel irritation. A smaller number face long-term issues months to years later. The goal is to weigh the risks of prostate cancer radiation therapy against its benefits. Techniques and spacers are employed to minimize healthy-tissue exposure and reduce serious harm.
Overview Of Radiation Therapy For Prostate Cancer
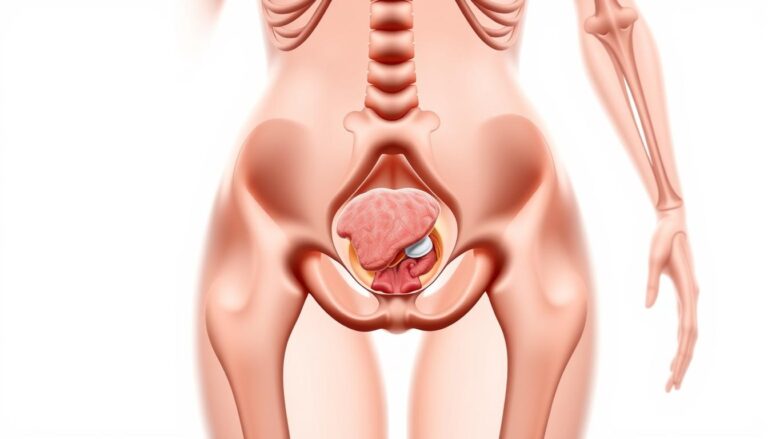
Radiation therapy is a key treatment for prostate cancer. It targets tumors with precision, aiming to damage cancer cells while sparing the rectum and bladder. Various methods are available, including external beams, seeds implanted in the gland, and radioisotopes that travel through the bloodstream.
What Radiation Therapy Is And How It Works
External beam therapy employs high-energy X-rays or photons to disrupt DNA in cancer cells. Proton therapy, on the other hand, uses charged particles that stop at a specific depth, minimizing damage beyond the prostate. Brachytherapy involves placing radioactive seeds or HDR sources inside the prostate, delivering a concentrated dose to nearby tissue.
Radiopharmaceuticals, like PSMA-targeted agents or bone-seeking isotopes, bind to tumor tissue, delivering radiation from within. Advanced planning uses CT and MRI scans to map the prostate and surrounding organs. Image-guided systems ensure daily treatments accurately target the planned area.
When Radiation Is Recommended In Prostate Cancer Care
For localized low- and intermediate-risk disease, radiation is often the first choice. In higher-risk cases, combining radiation with androgen-deprivation therapy can improve outcomes. After surgery, radiation may be recommended if pathology or rising PSA indicates remaining cancer.
For metastatic disease, targeted radiopharmaceuticals or focused external beams can alleviate pain and control symptoms at specific sites. The decision depends on disease extent, patient health, and treatment goals.
Common Goals: Cure, Adjuvant Therapy, Symptom Relief For Metastatic Disease
When disease is confined to the prostate, the primary goal is cure. Cure rates for selected patients are comparable to radical prostatectomy. Post-surgery, adjuvant or salvage radiation aims to reduce recurrence risk and manage rising PSA.
In advanced cancer, the focus shifts to symptom relief and disease control. Local treatments can alleviate urinary or rectal symptoms from pelvic tumors. Systemic radiopharmaceuticals aim to control spread and ease bone pain, with different side effects compared to local therapy.
Understanding radiation therapy side effects is essential for patients and clinicians. It helps weigh the benefits and risks of treatment. Awareness of complications, from pelvic toxicity to blood-count changes, guides treatment planning and follow-up care.
Types Of Radiation Therapy And How They Affect Side Effects
Different radiation therapies lead to varying side effects for patients. Each method aims to balance tumor control, convenience, and the risk to nearby organs. Knowing these differences is key to managing prostate cancer radiation side effects and setting realistic expectations.
External beam radiation therapy is a common choice. Modern techniques like IMRT, VMAT, and IGRT focus beams on the prostate while sparing the rectum and bladder. IMRT shapes the dose intensity to reduce hotspots. VMAT delivers similar plans faster as the machine rotates. IGRT uses imaging before each session to correct the prostate’s position. These advancements lower the risk of complications compared to older 3D conformal techniques. Treatments are typically given daily, five days a week, for several weeks. Hypofractionation shortens this course while maintaining effectiveness.
Stereotactic body radiation therapy delivers high doses in just a few sessions. Platforms like CyberKnife track motion and focus beams tightly. This method appeals due to fewer visits and a quicker overall treatment time. Some studies show higher rates of urinary or bowel symptoms in the short term. Long-term data are evolving, so clinicians must weigh the trade-offs when discussing side effects.
Brachytherapy places radioactive sources inside the prostate. Low-dose-rate implants using iodine-125 or palladium-103 emit low-dose radiation over weeks to months. High-dose-rate therapy uses temporary iridium-192 sources for brief treatments over days. Brachytherapy can cause more urinary irritation, which is worse in men with prior TURP or urinary issues. Rare risks include seed migration with LDR and the need for short radiation precautions after implantation.
Proton beam therapy uses charged particles that release most energy at a set depth, called the Bragg peak. This property can reduce dose beyond the prostate and may lower rectal or bladder exposure. Clinical outcomes have not shown clear superiority over top-tier photon techniques like IMRT for many patients. Limited availability and higher cost factor into decisions about using protons.
Radiopharmaceuticals deliver systemic radiation to prostate cancer cells or bone metastases. PSMA-targeted agents like 177Lu-PSMA-617 home in on tumor tissue and can cause fatigue, dry mouth, nausea, appetite changes, constipation, and blood count drops. Bone-directed drugs like radium-223 and other radionuclides concentrate in bone and can ease pain, with bone marrow suppression as a key risk. These therapies broaden the scope of radiation therapy complications for prostate cancer beyond local effects.
| Technique | Typical Schedule | Common Side Effects | Notes For Management |
|---|---|---|---|
| IMRT / VMAT / IGRT (EBRT) | Daily fractions, 4–9 weeks; hypofractionated regimens shorter | Urinary urgency, frequency, mild rectal irritation | Image guidance, rectal spacers, pelvic floor therapy |
| SBRT / SABR | 3–5 sessions over 1–2 weeks | Acute urinary flare, transient bowel symptoms | Careful patient selection, dose constraints, close follow-up |
| Brachytherapy (LDR / HDR) | LDR: single implant with ongoing emission; HDR: few fractions over days | Increased urinary irritation, rare seed migration, transient retention | Pre-treatment urologic assessment, catheter management, activity guidance |
| Proton Beam Therapy | Similar fractionation to EBRT; availability varies | Lower distal tissue dose; similar short-term urinary/bowel effects reported | Evaluate cost-access trade-offs, compare dose-volume metrics |
| Radiopharmaceuticals (PSMA, Bone Agents) | Systemic infusions; schedules depend on agent (weeks to months) | Fatigue, nausea, dry mouth, hematologic toxicity, marrow suppression | Blood count monitoring, symptom-directed care, hydration and nutrition |
Side Effects Of Radiation For Prostate Cancer
Radiation therapy for prostate cancer can alleviate symptoms while introducing a variety of side effects. Short-term symptoms often manifest during or shortly after treatment. Long-term complications may emerge months or even years later. Detailed descriptions are essential for patients and healthcare providers to assess risks and plan follow-up care.
Acute Versus Late Side Effects: Timeline And Typical Onset
Acute effects appear during treatment or shortly after its completion. Common symptoms include fatigue, urinary urgency, and frequency, as well as rectal irritation. Most of these symptoms improve with time and conservative management.
Late effects, on the other hand, emerge months to years post-treatment. These can include chronic radiation proctitis, persistent urinary incontinence, and urethral strictures. Understanding the timeline helps patients anticipate what to expect and when to seek specialized care.
How Dose, Technique, And Treated Area Influence Side Effects
The total dose and fraction size significantly impact normal-tissue injury. Higher doses and larger fractions, as seen in some SBRT programs, increase the risk of complications. Modern techniques like IMRT, IGRT, and MRI-linac focus the dose on the prostate, reducing common toxicities.
Combining external beam therapy with brachytherapy can improve tumor control but also increases genitourinary and bowel toxicity. Treating pelvic lymph nodes expands the radiation area, modestly raising risks like lymphedema and bowel upset.
Risk Factors That Increase Likelihood Or Severity Of Complications
Patient factors play a significant role in outcomes. Older age, pre-existing urinary symptoms, and a history of TURP increase urinary side effects. Active inflammatory bowel disease or prior pelvic surgery also raises bowel sensitivity. Smoking and high caffeine or alcohol intake exacerbate bladder and bowel symptoms.
Systemic agents like radiopharmaceuticals expose bone marrow and kidneys, altering the spectrum of complications. Kidney function, blood counts, and prior therapies are critical when assessing individual risks.
- Common but usually transient: urinary frequency, urgency, mild diarrhea, and fatigue.
- Gradual or late: erectile dysfunction, strictures, chronic proctitis, long-term incontinence.
- Uncommon but serious: severe strictures, persistent bleeding, rare secondary cancers.
Engaging in open discussions with a radiation oncologist and urologist is vital. It helps tailor treatment to individual goals while minimizing side effects. Prompt reporting of symptoms can significantly reduce long-term impacts.
Gastrointestinal Side Effects And Management
Managing bowel health during and after prostate radiation is both a science and an art. Men often experience changes in bowel habits, from mild urgency to visible bleeding. Early intervention and simple measures can alleviate symptoms and prevent long-term issues.
Radiation Proctitis: Symptoms, Causes, And Expected Course
Radiation proctitis occurs when the rectum receives unintended radiation due to its proximity to the prostate. Symptoms include rectal pain, urgency, frequent stools, mucus discharge, and bleeding. Acute cases often start during treatment and may improve weeks after therapy concludes. Chronic cases, appearing months to years later, may require specialist care for ongoing bleeding or leakage.
Diarrhea, Urgency, Rectal Bleeding, And Dietary Adjustments
Diarrhea and urgency are common side effects of pelvic radiation. Eating small, frequent meals and staying hydrated can help. Reducing high-fiber, spicy, and gas-producing foods can also alleviate symptoms. Patients are advised to limit caffeine, alcohol, and carbonated drinks, as they can irritate the gut.
For persistent diarrhea, loperamide may be prescribed. Topical treatments like sucralfate enemas or steroid protocols can help with bleeding. Severe or persistent bleeding should prompt a referral to gastroenterology or colorectal surgery.
Use Of Spacers, Medications, And Interventions To Reduce Bowel Toxicity
Technical measures can reduce rectal dose and protect the bowel. SpaceOAR hydrogel and balloon spacers increase the distance between the prostate and rectum, lowering exposure. Image-guided systems like IGRT and MRI-linac improve targeting and reduce errors.
For persistent bleeding, treatments such as argon plasma coagulation, formalin instillation, or hyperbaric oxygen may be considered. These are reserved for cases where conservative care has failed.
Effective management of radiation side effects requires a collaborative effort. Radiation oncologists, gastroenterologists, and colorectal surgeons work together to balance symptom relief with effective cancer treatment. This approach minimizes treatment interruptions and enhances daily comfort for patients.
| Symptom | Typical Timing | First-Line Management | Escalation Options |
|---|---|---|---|
| Urgency / Increased frequency | During treatment to weeks after | Diet change, hydration, loperamide | Pelvic floor therapy, specialist referral |
| Diarrhea | During treatment | Small meals, low-fiber choices, antidiarrheals | Review meds, stool studies, GI consult |
| Rectal bleeding | Acute or delayed (months to years) | Topical sucralfate, steroid enemas, iron if needed | Argon plasma coagulation, formalin, hyperbaric oxygen |
| Chronic proctitis with ulceration/stricture | Months to years after treatment | Specialist evaluation, symptom control | Surgical repair, stricturoplasty, long-term interventions |
| Prevention | Before and during planning | SpaceOAR or balloon spacer, IGRT, MRI-linac planning | Adaptive planning, dose modification |
Urinary Side Effects And Long-Term Risks
Radiation to the pelvic area can irritate the bladder and nearby tissues. Men often notice new urinary habits during or after treatment. Clinicians discuss risks up front so patients can prepare and manage symptoms effectively.
Radiation Cystitis: Frequency, Urgency, Dysuria, And Hematuria
Radiation cystitis is bladder inflammation from pelvic radiation. Symptoms include increased frequency, sudden urgency, burning with urination (dysuria), and sometimes visible blood in the urine (hematuria).
Many men see symptoms during treatment that ease afterward. A minority develop chronic cystitis that persists or returns months later. Care teams rule out infection, monitor hematuria, and offer treatments to control bleeding and pain.
Urinary Incontinence And Urethral Stricture — Presentation And Treatments
Severe incontinence is less common after radiation than after radical prostatectomy, yet leakage and urgency can occur. Symptoms range from mild dribbling to more disruptive daily issues.
Urethral stricture is a narrowing that may appear months or years after therapy. Men may report a weak stream, trouble starting, urinary retention, or repeated infections. Simple dilation or internal urethrotomy often helps. Complex cases can need surgical reconstruction.
Medical treatments include alpha-blockers, anticholinergics, and antispasmodics. Pelvic floor exercises and bladder training support recovery. For significant bleeding, cystoscopy, cautery, bladder irrigation, or interventional radiology may be required.
Preparing The Bladder During Planning And Strategies To Reduce Exposure
During simulation and daily sessions, a consistent bladder filling protocol is common. A moderately full bladder lifts the small bowel and stabilizes prostate position. This practice reduces dose to bladder and bowel and limits radiation therapy for prostate cancer side effects.
Advanced imaging tools such as IGRT and MRI-linac tighten margins and cut unintended exposure. Spacers and careful contouring further protect tissues. Pre-treatment counseling about existing urinary problems, prior TURP, and prostate size helps tailor plans and lower long-term risk.
| Issue | Typical Onset | Common Management | When To Escalate Care |
|---|---|---|---|
| Radiation cystitis (frequency, urgency, dysuria) | During treatment to early post-treatment | Hydration, antispasmodics, alpha-blockers, pelvic floor exercises | Severe pain or persistent symptoms beyond weeks |
| Hematuria (bladder bleeding) | During or weeks to months after therapy | Evaluate for infection, cystoscopy, bladder irrigation, endoscopic cautery | Recurrent or heavy bleeding, anemia, clot retention |
| Urinary incontinence | Weeks to months after treatment | Pelvic floor rehab, absorbent products, medications | Severe lifestyle impact; consider urology referral for procedures |
| Urethral stricture | Months to years later | Dilation, internal urethrotomy, surgical reconstruction | Recurrent retention, infections, failed endoscopic therapy |
| Pre-existing urinary symptoms | Present before treatment | Optimize BPH care, consider TURP or medications before radiation | Worsening symptoms despite optimization |
Clear discussion about urinary side effects of radiation and practical steps for coping with radiation side effects helps men make informed choices. Early reporting of symptoms speeds treatment and improves outcomes.
Sexual Health And Fertility After Radiation Therapy
Radiation for prostate cancer impacts more than just PSA levels. It can significantly alter sexual function and fertility, with effects unfolding over months to years. Providing clear, practical information is essential for patients and their partners to plan care and preserve options.
Erectile decline often becomes apparent only after a period of time. Unlike surgery, where immediate loss of function is common, radiation-related erectile dysfunction develops gradually. This gradual onset contrasts with the immediate effects seen after radical prostatectomy.
Age and the initial strength of erections play a significant role in determining risk. Studies indicate that long-term erectile dysfunction rates after radiation therapy are similar to those after surgery. Individual outcomes are influenced by factors such as radiation dose, technique, and overall health.
Ejaculation and semen quality also undergo changes. Radiation can lead to a decrease in ejaculate volume, potentially resulting in a dry or absent ejaculation over time. Both external beam radiation and brachytherapy can cause these effects, with the timing typically gradual.
Fertility is a critical concern for younger men undergoing radiation therapy. Pelvic radiation and certain radiopharmaceuticals can impair sperm production and function. Sperm banking before treatment is a viable option for those considering biological children in the future.
Practical steps can enhance recovery and quality of life. Early consultation with a urologist, fertility specialist, or reproductive clinic facilitates sperm banking and preservation. Proactive rehabilitation, such as trying PDE5 inhibitors, can also support long-term sexual function.
Treatment options for sexual dysfunction range from medical to device-based interventions. Common initial treatments include sildenafil and tadalafil. Vacuum erection devices and intracavernosal injections are considered when pills are ineffective. Penile implants offer a durable solution for those with persistent issues.
Emotional and relationship aspects are equally important. Counseling, sexual therapy, and couple-based support can ease the transition and improve treatment adherence. Early referral to specialists is key to achieving better outcomes.
| Issue | Typical Timeline | Common Interventions | Fertility Note |
|---|---|---|---|
| Erectile Dysfunction | Months to years after radiation | PDE5 inhibitors, vacuum device, injections, implant | No direct effect on sperm banking; fertility may decline |
| Changes In Ejaculation | Gradual reduction in semen volume | Expectant management, fertility referral if desired conception | Sperm retrieval may be needed for assisted reproduction |
| Fertility Risk | Immediate and long-term depending on dose | Sperm banking, consult reproductive urology | Radiopharmaceuticals can also impair fertility |
| Psychosexual Impact | Concurrent with physical changes | Cognitive-behavioral therapy, couples counseling, sex therapy | Partner involvement improves planning and outcomes |
- Discuss sperm banking before starting treatment when future fertility matters.
- Expect sexual side effects of radiation for prostate cancer to be progressive; set realistic goals early.
- Include prostate cancer radiation side effects management in follow-up plans with urology and sexual health teams.
Systemic And Other Side Effects From Advanced Or Targeted Radiotherapies
Advanced radiation therapies offer benefits but also introduce new side effects. Patients often experience systemic symptoms that differ from traditional pelvic reactions. Effective monitoring and supportive care plans are essential for managing daily life and long-term health.
Fatigue: Causes, Duration, And Energy-Management Strategies
Fatigue is a common complaint during and after treatment. It can start during external beam therapy or after a dose of a radiopharmaceutical. Symptoms may last for weeks to months.
Several factors contribute to tiredness. These include low-grade inflammation, drops in blood counts, disturbed sleep, and a cycle of reduced activity. Practical steps can help manage radiation side effects. These include conserving energy, taking short walks, maintaining consistent sleep routines, and eating balanced meals.
Hematologic Effects And Kidney Risks With Radiopharmaceuticals
PSMA-targeted agents like 177Lu-PSMA-617 can lower red cells, platelets, and white cells. This increases the risk of anemia, infection, and bleeding. Regular blood counts are essential for adjusting doses and supportive care.
Some radiopharmaceuticals can harm the kidneys. To mitigate this, patients should stay hydrated before and after infusions. Baseline kidney function tests and ongoing monitoring are also necessary. Communication between nuclear medicine, medical oncology, and urology is key to early problem detection and therapy adjustments.
Lymphedema After Nodal Irradiation And Physical Therapy Approaches
Treatment of pelvic lymph nodes can slow lymph flow. This leads to swelling in the legs or genital area, often appearing months after therapy. Lymphedema can improve but may persist.
Effective treatments focus on drainage and strengthening. Manual lymphatic drainage, compression garments, and targeted exercises help reduce fluid buildup. Early referral to a lymphedema therapist is critical for effective management.
Radiation Skin Reactions And Rare Secondary Malignancy Risk
Skin in the treatment field may redden or peel, similar to a sunburn. Mild soap, petroleum-based moisturizers, and loose clothing can help manage discomfort. Severe cases require wound care from dermatology or radiation oncology.
There is a very low but real risk of secondary cancers in irradiated tissue years later. This risk is weighed against the benefits of cancer control. Patients on systemic agents must follow safety precautions due to temporary radioactivity in body fluids. Hydration and avoiding close contact with young children or pregnant visitors are common precautions.
Monitoring And Multidisciplinary Care
Routine labs and kidney checks are standard for patients on systemic agents. Teams including radiation oncologists, nuclear medicine specialists, urologists, and oncology nurses coordinate surveillance and symptom management.
Open communication and early symptom reporting are essential for improving outcomes. This approach minimizes the impact of radiation therapy complications for prostate cancer. It also supports practical strategies for managing radiation side effects and addressing radiopharmaceutical side effects as they arise.
Managing Radiation Therapy Side Effects And Improving Quality Of Life
The journey after prostate radiation therapy requires a collaborative effort and small, daily decisions. A well-thought-out plan for managing side effects is key to staying active and feeling in control. This involves multidisciplinary care and practical self-care strategies.
Radiation oncologists work closely with urologists, nurses, dietitians, and other specialists. Regular check-ups monitor PSA levels, urinary and bowel function, sexual health, and blood counts. This team-based approach makes managing side effects more effective and tailored to each patient’s needs.
Specific treatments address various symptoms. For example, medications and procedures help with bowel and urinary issues. In cases of persistent rectal bleeding, treatments like argon plasma coagulation or hyperbaric oxygen are considered. Severe blood-related problems might require transfusions or other forms of support.
Pelvic floor physical therapy is beneficial for reducing leakage and aiding recovery. Therapists teach exercises and biofeedback to help. Sexual health specialists offer treatments like oral medications or vacuum devices, and may refer patients for penile rehabilitation. Sperm banking is an option for those who wish to preserve fertility.
Adopting a healthy diet and lifestyle can alleviate symptoms. Drinking plenty of water, avoiding certain foods and drinks, and eating small, low-residue meals can help. With PSMA agents, increasing fluid intake and frequent voiding protect the bladder.
Simple routines can significantly improve daily life. Maintaining a consistent bladder-filling routine, using incontinence pads if needed, and quitting smoking are all helpful. Open communication about sexual changes with partners and healthcare providers is also essential for emotional support.
Knowing when to seek urgent care is critical. Symptoms like high fever, heavy bleeding, inability to urinate, sudden severe swelling, chest pain, or shortness of breath require immediate attention. Severe infections in patients with low white blood cell counts are emergencies. At routine visits, report any new or worsening symptoms, including urinary or bowel issues, erectile dysfunction, fatigue, or signs of hematologic or renal decline.
| Issue | First-Line Self-Care | Clinician Options |
|---|---|---|
| Diarrhea / Urgency | Hydration, low-residue diet, psyllium, loperamide | Antispasmodics, topical rectal therapy, dietary counseling |
| Urinary Frequency / Dysuria | Fluid timing, avoid caffeine/alcohol, bladder training | Alpha-blockers, antimuscarinics, referral to urology |
| Rectal Bleeding | Avoid NSAIDs, soft diet, monitor blood loss | Argon plasma coagulation, formalin, hyperbaric oxygen |
| Urinary Incontinence | Pelvic floor exercises, pads, timed voiding | Pelvic floor physical therapy, pessary or surgical options |
| Fatigue | Short walks, balanced meals, sleep hygiene | Assess for anemia, treat reversible causes, rehab programs |
| Sexual Dysfunction | Open partner communication, devices, PDE5 trials | Medications, penile rehabilitation, referral to sexual health clinic |
Conclusion
Radiation therapy is a significant treatment for prostate cancer, encompassing curative external beam methods like IMRT and VMAT, as well as targeted brachytherapy and radiopharmaceuticals. Each method effectively controls the disease. Yet, the side effects of radiation for prostate cancer span various domains, including urinary, bowel, sexual, and systemic. These effects depend on the dose, technique, and patient’s health.
Modern tools such as IGRT, MRI-linac, rectal spacers, and meticulous treatment planning help minimize collateral damage. Brachytherapy, with its steep dose fall-off, further limits exposure. Radiopharmaceuticals, though, extend care to metastatic disease but introduce complications like hematologic or renal effects that require monitoring.
Most side effects from radiation therapy are temporary and can be managed with dietary changes, medications, pelvic floor therapy, and coordinated care from urologists and radiation oncologists. Some issues, such as erectile dysfunction, strictures, chronic proctitis, or lymphedema, may arise later and necessitate specialist intervention.
Choosing the right treatment involves weighing the benefits against the risks for each individual. It’s essential to discuss baseline bladder and bowel function, fertility plans, and lifestyle with the care team. Taking proactive steps like bladder protocols, spacers, sperm banking, and early rehabilitation, along with regular follow-up, can enhance quality of life and long-term outcomes post-prostate cancer treatment.
FAQ
What Is Radiation Therapy For Prostate Cancer And How Does It Work?
Radiation therapy employs high-energy X-rays, proton beams, or radioactive drugs to damage cancer cells’ DNA. This prevents them from dividing. External beam machines (linacs) direct beams from outside the body. Proton centers use particle accelerators to precisely place the dose at the tumor site. Brachytherapy implants radioactive seeds or temporary HDR sources inside the prostate. Radiopharmaceuticals, like lutetium Lu 177 vipivotide tetraxetan (Pluvicto), target tumor cells through the bloodstream.
Planning involves CT or MRI scans. Techniques like IMRT, IGRT, VMAT, SBRT, and MRI‑linac shape and aim the dose. This minimizes damage to the rectum, bladder, and surrounding tissue.
When Is Radiation Recommended In Prostate Cancer Care?
Radiation is a primary treatment for many men with localized prostate cancer. It’s often combined with androgen-deprivation therapy for higher-risk cases. After prostatectomy, radiation may be used as adjuvant or salvage treatment.
In cases of metastatic disease, external beam or radiopharmaceuticals help manage symptoms and control systemic disease.
What Are The Main Types Of Radiation And How Do Side Effects Differ?
External beam radiation (EBRT) uses IMRT/VMAT/IGRT to sculpt the dose, reducing rectal and bladder exposure. This tends to have predictable urinary and bowel effects. SBRT/SABR delivers larger doses in fewer sessions, sometimes causing higher acute symptoms.
Brachytherapy gives localized high doses, with risks like urinary irritation or seed migration. Proton therapy may reduce dose beyond the target but lacks clear clinical superiority. Radiopharmaceuticals cause systemic effects like fatigue and blood-count changes, not localized pelvic toxicity.
What Are The Typical Acute And Late Side Effects To Expect?
Acute side effects include fatigue, urinary urgency or frequency, dysuria, diarrhea, and rectal irritation. These symptoms appear during treatment and in the weeks after. Late effects may develop months to years later, including chronic radiation proctitis, bladder problems, and erectile dysfunction.
Many acute symptoms improve with time, but a minority experience long-term complications.
How Do Dose, Technique, And Treated Area Affect Risk Of Complications?
Higher total doses and larger fraction sizes increase normal-tissue toxicity risk. Advanced techniques like IMRT, IGRT, and MRI-linac reduce side effects. Treating pelvic lymph nodes raises lymphedema risk.
Combining EBRT with brachytherapy increases genitourinary and bowel toxicity. Individual risk is shaped by baseline urinary or bowel disease and prior pelvic procedures.
What Is Radiation Proctitis And How Is It Managed?
Radiation proctitis is rectal inflammation from incidental rectal dose. Symptoms include urgency, more frequent bowel movements, mucus or rectal bleeding, and pain. Acute proctitis usually improves after treatment.
Chronic proctitis can cause ongoing bleeding or leakage. Management ranges from dietary changes and antidiarrheals to topical sucralfate, steroid enemas, and argon plasma coagulation for bleeding. Spacers and precise imaging help prevent severe rectal dose.
What Dietary And Lifestyle Steps Reduce Bowel Symptoms During Treatment?
Simple adjustments help: avoid spicy, high-fiber, gas-producing foods, reduce caffeine and alcohol, eat small frequent low-residue meals, and stay well hydrated. Antidiarrheals such as loperamide can control urgent diarrhea.
Discuss a tailored diet plan with the care team or dietitian to manage symptoms during pelvic radiation.
What Urinary Side Effects Should Patients Expect And How Are They Treated?
Bladder irritation (radiation cystitis) often causes frequency, urgency, painful urination, and sometimes hematuria during or shortly after treatment. Most improve over weeks to months. Treatments include alpha-blockers, antispasmodics, pelvic floor therapy, bladder irrigation or cystoscopic cautery for bleeding.
In severe cases, interventional radiology or surgery may be necessary. Urethral strictures and persistent incontinence can appear months to years later and may require dilation, urethrotomy, or reconstructive surgery.
How Should Patients Prepare Their Bladder For Planning And Treatments?
Consistent bladder filling is usually requested at simulation and each treatment—a moderately full bladder—to push small bowel away and stabilize prostate position. Following the center’s specific instructions improves targeting and reduces bladder and bowel dose. IGRT and MRI-linac imaging further refine daily setup.
How Does Radiation Affect Sexual Function And Fertility?
Erectile dysfunction after radiation typically develops gradually over months to years. Long-term ED rates are similar to surgery in many studies but vary by age and baseline function. Radiation also reduces semen volume and can cause dry ejaculation.
Pelvic radiotherapy and radiopharmaceuticals can cause infertility; men who want future biological children should consider sperm banking before treatment.
What Are Treatment Options For Radiation‑Related Erectile Dysfunction?
First-line therapies include phosphodiesterase-5 inhibitors (sildenafil, tadalafil), vacuum erection devices, and pelvic floor or sexual counseling. Intracavernosal injections and penile implants are options for refractory cases. Early discussion with urology and sexual health specialists and couple support improves outcomes.
What Systemic Side Effects Are Associated With Radiopharmaceuticals Like Pluvicto?
PSMA-targeted agents such as 177Lu-PSMA-617 commonly cause fatigue, dry mouth, nausea, appetite changes, constipation, and hematologic toxicity—anemia, thrombocytopenia, and neutropenia. Bone-directed isotopes (radium-223) relieve pain from bone metastases but can suppress marrow. Clinicians monitor blood counts and kidney function and advise hydration to reduce renal risk.
How Common Is Fatigue And How Can Patients Manage It?
Fatigue is very common during and after both EBRT and systemic radiopharmaceuticals. It may begin during treatment and last weeks to months. Management includes graded exercise, energy conservation, good sleep habits, balanced nutrition, and treating reversible causes such as anemia.
Occupational therapy and counseling support can help maintain daily function.
What Is Lymphedema After Pelvic Irradiation And How Is It Treated?
Lymphedema can occur when pelvic lymph nodes are treated—resulting in leg or genital swelling due to impaired lymph drainage. Management focuses on manual lymphatic drainage, compression garments, specialized physical therapy, exercise, and skin care. Early referral to lymphedema specialists improves outcomes, though symptoms may persist.
What Monitoring And Follow‑Up Are Needed After Radiopharmaceuticals?
Regular blood tests to check blood counts and renal function are essential after systemic agents. Follow-up visits monitor PSA, urinary and bowel function, fatigue, and any signs of infection or bleeding. Multidisciplinary coordination between radiation oncology, nuclear medicine, urology, and primary care ensures early detection and management of toxicities.
What Multidisciplinary Support And Therapies Help Manage Side Effects?
Optimal care blends radiation oncologists, urologists, nurses, dietitians, pelvic floor and physical therapists, sexual health specialists, and primary care. Interventions include medications (antidiarrheals, alpha-blockers, antispasmodics), pelvic floor rehabilitation, dietary counseling, spacers at planning, topical or endoscopic treatments for proctitis, blood transfusion or hematologic support for cytopenias, and psychosocial support.
What Practical Self‑Care Steps Reduce Symptoms During And After Treatment?
Practical tips include staying hydrated (often about 2 liters/day unless advised differently), following bladder-filling instructions, avoiding smoking, cutting caffeine and alcohol, using incontinence products if needed, following a gentle diet, and starting pelvic floor exercises. Communicating new or worsening symptoms to the care team enables timely management.
When Should Patients Seek Urgent Care During Or After Radiation?
Seek urgent care for high fever, severe bleeding, inability to urinate, sudden marked swelling or signs of lymphedema complications, chest pain or shortness of breath, or severe infection signs in the setting of low white blood cell counts. Any rapid change in urinary retention, persistent severe rectal bleeding, or suspected sepsis requires immediate attention.
How Should Patients Discuss Risks And Trade‑Offs With Their Team Before Treatment?
Men should discuss baseline urinary and bowel function, prior pelvic surgeries (like TURP), prostate size, fertility desires, lifestyle and work needs, and tolerance for short- versus long-term risks. Ask about options to reduce toxicity—spacers, IMRT/IGRT, hypofractionation vs. conventional schedules—and what follow-up and rehabilitation support will be available. Personalized counseling helps balance cure rates, quality of life, and long-term side-effect risk.