The Truth About Prostate Biopsy: Risks and Benefits
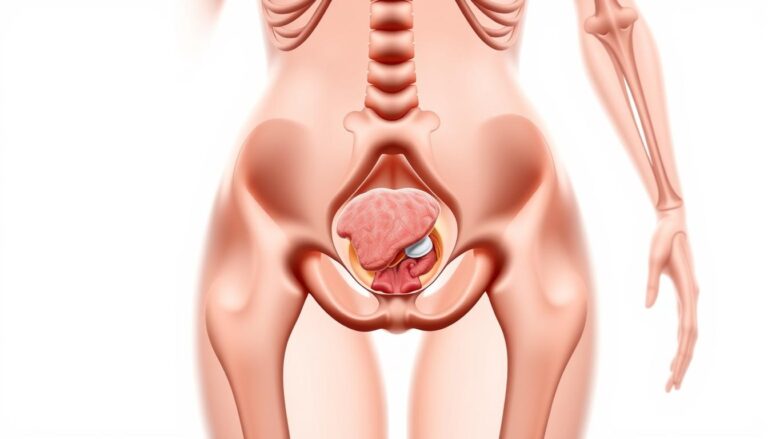
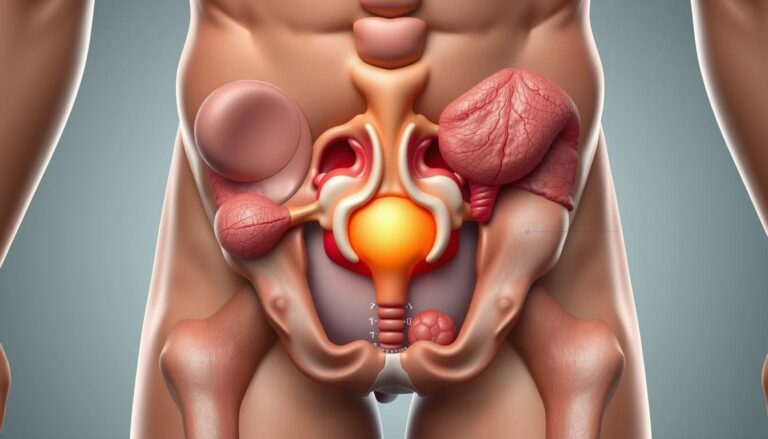
The prostate, a small, walnut-shaped gland, is located beneath the bladder. It plays a key role in making seminal fluid and encases the urethra. If prostate cancer screening reveals a high PSA or an unusual finding on a digital rectal exam, a biopsy is often recommended. This procedure samples tissue to confirm if cancer is present and its aggressiveness.
A biopsy provides a definitive diagnosis, guiding treatment options from active surveillance to surgery or radiation. Before the procedure, a urologist typically conducts urine tests to rule out infection. They may also use multiparametric MRI to pinpoint suspicious areas.
Considering the risks and benefits of a prostate biopsy involves making a trade-off. It can detect significant cancers needing treatment but may also identify slow-growing tumors, leading to overdiagnosis and anxiety. Short-term complications like bleeding, infection, and urinary retention are possible. The accuracy of the biopsy can vary based on the technique used.
This article presents the truth about prostate biopsy as a careful trade-off. It is an essential diagnostic tool with clear value but not without its limits. The following sections will explore how biopsies work, what the results mean, and how to balance risks and benefits when deciding on the next steps after screening.
What Is A Prostate Biopsy And Why It’s Done
A prostate biopsy is a precise method to collect tiny samples of prostate tissue for lab analysis. The prostate, located below the bladder and around the urethra, plays a role in seminal fluid production. A urologist uses a thin, spring-loaded needle to extract several small cores during the procedure. These samples are then examined by a pathologist to detect cancer or other abnormalities.
Definition And Basic Anatomy Of The Prostate
The prostate, roughly the size of a walnut in younger men, can grow with age. It encircles the urethra, which is why prostate issues often impact urination. The tissue cores obtained during a biopsy provide direct evidence of cellular changes. These samples are essential for pathology reports that identify cancer, inflammation, or premalignant lesions.
Common Indications: Elevated PSA And Abnormal Digital Rectal Exam
Doctors may recommend a biopsy if PSA levels persistently rise or if a digital rectal exam reveals a nodule or irregularity. Other reasons include a repeat increase in PSA after a benign biopsy or the presence of atypical cells. Routine urine tests are conducted to exclude infection before the biopsy. These steps are part of the standard prostate cancer screening process aimed at detecting clinically significant disease.
How Biopsy Informs Diagnosis, Staging, And Treatment Planning
Pathologists analyze the cores to determine if cancer is present and assign a grade that forecasts its behavior. The Gleason score or Grade Group, derived from the biopsy, guides prognosis and treatment options. Combining biopsy results with imaging and exam findings helps determine staging and treatment plans. For some, this may lead to active surveillance, while others may require surgery, radiation, or other therapies.
The Truth About Prostate Biopsy
A prostate biopsy often raises more questions than answers. Short bursts of discomfort are common during a TRUS procedure that takes about 20 minutes. Local anesthesia numbs the area and most men feel only brief pressure when cores are taken.
Separating Facts From Fears About The Procedure
Prostate biopsy facts show that minor aftereffects are typical. Expect some rectal bleeding, blood in the urine or semen, and soreness for a few days. Serious events such as sepsis or urinary retention happen but are uncommon when antibiotics and standard precautions are used.
How Biopsy Results (Pathology And Gleason Scoring) Affect Decisions
Pathology reports describe tissue samples and cell patterns. Gleason scoring combines the two most common patterns to produce a score from 6 to 10. A Gleason 6 is low-grade, 7 is intermediate, and 8–10 are high-grade. These grades steer choices about monitoring or active treatment.
Overdiagnosis And Why Not All Detected Cancers Need Immediate Treatment
Many prostate biopsy facts reveal that random sampling can find tiny, slow-growing tumors. Up to half of detected cancers may be clinically insignificant. This leads to worries about overtreatment and side effects such as incontinence or erectile dysfunction.
Decisions rest on age, overall health, PSA trends, MRI findings, and Grade Group. Active surveillance is a common path for low-risk disease. It reduces unnecessary treatment while keeping a watchful eye on change.
Readers should weigh the truth about prostate biopsy and the risks of prostate biopsy alongside benefits. Discuss options with a urologist from centers like Mayo Clinic or Cleveland Clinic.
Types Of Prostate Biopsy Procedures And How They Differ
Prostate biopsy procedures vary in terms of accuracy, comfort, and infection risk. Healthcare providers consider patient history, MRI results, and available technology when deciding. This section outlines three common methods and their differences in practice.
Transrectal Ultrasound-Guided Technique And Workflow
The TRUS biopsy is the most common method used in many clinics. An ultrasound probe is inserted into the rectum to guide a needle into the prostate. This process involves 10–12 systematic cores taken in about 20 minutes.
Its strengths include widespread availability and a proven track record, surpassing PSA testing alone. Yet, it has limitations. Blind sampling can miss anterior lesions, leading to false-negative rates near 30% in some cases.
Transperineal Approach: Timing, Targeting, And Imaging Support
Transperineal biopsy accesses the gland through the skin between the anus and scrotum. Needles pass through the perineum, often under local or general anesthesia. MRI or CT guidance can enhance precision.
This method offers better access to anterior and transition zones, reducing infection risk from rectal flora. Urologists often prefer it for repeat biopsies or when MRI shows anterior lesions.
MRI-Targeted Techniques And Fusion Versus Systematic Sampling
Multiparametric MRI highlights suspicious targets invisible to ultrasound. MRI-targeted biopsy can be cognitive, use MRI-ultrasound fusion, or occur inside the MRI bore.
Targeted cores improve detection of clinically significant cancer, often reducing unnecessary sampling. Many centers combine targeted cores with systematic sampling to ensure no disease is missed.
| Method | Typical Guidance | Sample Count | Strengths | Limitations |
|---|---|---|---|---|
| TRUS biopsy | Transrectal ultrasound | 10–12 cores | Widely available; quick; familiar workflow | Blind to some lesions; higher rectal-flora infection risk |
| Transperineal biopsy | Transperineal access with ultrasound, MRI, or CT | Variable; targeted plus systematic common | Better anterior access; lower infection risk; good for repeat biopsies | Often needs more anesthesia and specialized setup |
| MRI-targeted biopsy | Multiparametric MRI with cognitive, fusion, or in-bore sampling | Targeted cores, often combined with systematic cores | Higher detection of significant cancers; fewer unnecessary cores | Requires MRI access and fusion expertise; cost and availability vary |
Clinical decisions hinge on imaging access, operator skill, and patient factors. Some teams opt for MRI-targeted biopsy with systematic sampling for better precision and coverage. The choice of procedure is influenced by equipment investments and training.
What To Expect During A Prostate Biopsy Procedure
A prostate biopsy is a brief, focused visit that combines simple preparation with precise sampling. Patients receive clear instructions a week before. The staff explains each step to avoid surprises. The goal is to collect tissue efficiently with minimal discomfort.
Preparation Steps: Urine Tests, Antibiotics, Medication Adjustments, Enemas
Before the procedure, a urine test checks for infection. If a urinary tract infection appears, the biopsy is postponed until antibiotics clear it. Urologists often prescribe a short antibiotic course as prophylaxis to reduce infection risk.
Patients stop blood-thinning medicines such as warfarin, aspirin, or NSAIDs several days before the biopsy to lower bleeding risks. A cleansing enema may be suggested on the morning of the procedure. These measures are standard prostate biopsy preparation used in clinics across the United States.
Procedure Positioning, Ultrasound Probe Use, Local Anesthesia, Core Sampling
For a TRUS-guided approach, the patient lies on the side with knees drawn up or occasionally lies prone. The rectal area is cleaned and a lubricating gel applied. An ultrasound probe enters the rectum to map the prostate and guide needle placement.
Local anesthetic injections numb the prostate and perineum. A spring-loaded biopsy gun then captures thin cylindrical tissue samples. Each pass yields a brief sting. The process of biopsy core sampling focuses on getting representative tissue from different prostate zones.
Typical Duration And Number Of Tissue Cores Taken
The clinic visit usually lasts an hour, while the active biopsy runs about 10–20 minutes. A standard systematic TRUS biopsy collects roughly 10 to 12 cores. If MRI shows a suspicious lesion, technicians add targeted cores to improve detection of clinically important tumors.
| Step | What Happens | Typical Timing |
|---|---|---|
| Pre-procedure Screening | Urine test, medication review, antibiotic plan, optional enema | 1–7 days before |
| Positioning And Imaging | Side-lying or prone position, ultrasound probe inserted, prostate mapped | 5–10 minutes |
| Anesthesia | Local injections to numb the prostate and nearby tissue | 2–5 minutes |
| Biopsy Core Sampling | Spring-loaded gun retrieves thin tissue cores; typically 10–12 systematic cores, plus targeted cores if needed | 5–15 minutes |
| Recovery And Aftercare | Brief monitoring, written aftercare instructions, short antibiotic course in many cases | 15–30 minutes |
After the biopsy, light activity is advised for 24–48 hours. Expect some temporary bleeding in urine, stool, or semen. Most symptoms fade within a few days. Clear communication with the clinic makes the process smooth and predictable for patients wondering what to expect during prostate biopsy.
Risks Of Prostate Biopsy
A prostate biopsy offers clear benefits but also comes with some downsides. It’s important to understand the common aftereffects, how to prevent infection, and which rare problems require immediate medical attention.
Common Short-Term Effects
Rectal bleeding is a common side effect of transrectal biopsy, usually mild. Blood in the urine, or hematuria, may last a few days. Blood in semen, or hematospermia, can persist for weeks, causing more concern than harm.
Infection Risk And Antibiotic Use
The biopsy can introduce bacteria from the rectum into the prostate or bloodstream. This can lead to urinary tract infections or, rarely, sepsis. To mitigate this, antibiotics are given before the biopsy. Urine tests are done beforehand to treat any existing infections.
Urinary Retention And Urgent Complications
Some men may struggle to urinate after the biopsy. In severe cases, a temporary catheter is needed. Severe pain, prolonged heavy bleeding, fever, or chills are urgent signs that require immediate medical attention.
How Technique Changes Risk
The choice of biopsy technique impacts the risk of complications. The transperineal method is associated with lower infection rates compared to the transrectal method. This is a consideration for healthcare providers when deciding on the procedure.
When To Call A Doctor
If you experience fever over 100.4°F, worsening pain, inability to urinate, or heavy bleeding, seek medical attention. Studies suggest that complications like infection, bleeding, or severe pain occur in about three to seven percent of cases. Being vigilant can help identify issues early.
Benefits Of Prostate Biopsy
A prostate biopsy transforms a vague test result into a detailed tissue analysis. For men with elevated PSA levels or suspicious physical exams, it offers more than just numbers. It provides real tissue samples for pathologists to examine, leading to a definitive diagnosis and actionable steps.
Definitive Tissue Diagnosis And Ability To Grade Cancer Aggressiveness
Through biopsy tissue, labs can confirm if abnormal cells are cancerous or benign, like prostatitis. Pathologists then identify the tumor type and assess its aggressiveness. This information is critical for understanding the cancer’s prognosis. The biopsy also yields a Gleason score or Grade Group, which indicates the cancer’s aggressiveness under the microscope.
Guiding Appropriate Treatment: Active Surveillance Versus Definitive Therapy
Biopsy results are key in making significant treatment decisions. For men with low-grade disease, active surveillance might be the best option, avoiding the side effects of surgery or radiation. On the other hand, higher-grade findings often necessitate definitive therapy, which can significantly improve long-term outcomes.
How Biopsy Can Identify Clinically Significant Cancers That Need Intervention
Advanced techniques like MRI-targeted and transperineal sampling enhance the detection of significant tumors. These methods help identify prostate cancer that requires immediate attention while sparing men from unnecessary treatments for slow-growing lesions. In essence, biopsy helps distinguish between cancers that need urgent treatment and those that can be monitored.
The benefits of prostate biopsy are clear: it provides a definitive diagnosis, grading that guides treatment, and the ability to detect significant prostate cancer. These results enable doctors to tailor care to each patient’s risk, eliminating the need for guesswork.
Prostate Biopsy Accuracy, Limitations, And False Negatives
Prostate biopsy accuracy varies based on the technique used and the prostate’s anatomy. Many urologists agree that a standard 12-core transrectal ultrasound-guided (TRUS) biopsy can miss significant disease. This reality leads to repeat testing and alternative methods when clinical suspicion remains high.
Systematic TRUS sampling has modest sensitivity in some studies. Reports indicate sensitivity near 50–53% for detecting all tumor foci. False-negative rates can reach roughly 30% in selected series. This explains why a single negative biopsy does not always end the diagnostic conversation.
Random core sampling can miss tumors that are small or located in the anterior parts of the gland. Large prostates, operator technique, and heterogeneous tumor patterns increase the risk of false negatives. Atypical histology or rising PSA after a negative biopsy often prompts reconsideration.
When clinical signs persist, repeating the biopsy makes sense. Many clinicians turn to targeted methods such as transperineal mapping or MRI-guided cores. These approaches improve detection of clinically important cancer and reduce unnecessary sampling.
Multiparametric MRI is increasingly important in narrowing misses. It highlights suspicious regions, helping teams plan targeted or fusion biopsies. This combination enhances detection of aggressive lesions while reducing false negatives.
In practice, combining imaging and targeted sampling yields better prostate biopsy accuracy than systematic TRUS alone. Shared decision-making, attention to PSA trends, and repeat testing when warranted help ensure cancers are not overlooked.
Comparing Prostate Biopsy Vs. MRI In Screening And Diagnosis
Deciding between imaging and tissue sampling is akin to selecting the right map for a journey. Multiparametric MRI serves as a satellite view, pinpointing suspicious areas without invasive procedures. Despite MRI’s ability to guide biopsies, tissue sampling remains the definitive diagnostic tool. It provides a detailed look at the tissue, essential for accurate diagnosis.
Strengths And Limits Of MRI As A Noninvasive Diagnostic Tool
Prostate cancer screening MRI uses various sequences to highlight lesions, aiding in risk stratification and tumor detection. Radiology centers, like Mayo Clinic, report that MRI reduces false positives and clarifies when further testing is necessary.
While MRI is invaluable, it cannot replace histological examination. Visible lesions require biopsy to confirm cancer and assess aggressiveness. The effectiveness of MRI in routine care depends on availability, cost, and the radiologist’s expertise.
When MRI Can Guide Targeted Biopsy And Reduce Unnecessary Cores
MRI-targeted biopsy allows clinicians to precisely target suspicious lesions. Techniques include cognitive targeting, ultrasound-MRI fusion, and in-bore MRI sampling. This focused approach increases the likelihood of detecting significant cancer while minimizing unnecessary cores.
Practices employing MRI-targeted biopsy report fewer repeat procedures and clearer treatment pathways. This method streamlines decision-making, improving patient outcomes.
Combined Strategies: MRI Fusion Biopsy And Clinical Decision Pathways
Many urology programs integrate MRI with systematic sampling to balance detection and overdiagnosis. Fusion biopsies combine MRI maps with real-time ultrasound, ensuring thorough examination of both obvious lesions and the rest of the gland.
Clinical pathways now consider PSA trends, MRI results, and patient health before deciding on biopsy or MRI-first approaches. Guidelines increasingly support MRI before repeat biopsy, when feasible and affordable, to enhance decision-making.
- Pros of prostate cancer screening MRI: noninvasive risk stratification, fewer unnecessary biopsies.
- Pros of biopsy: definitive histology, grading for treatment planning.
- Best practice often blends both: MRI-targeted biopsy plus selective systematic cores.
Interpreting Prostate Biopsy Results And What They Mean For Patients
A pathology report transforms small tissue samples into a detailed medical narrative. It outlines a gross description, microscopic cell details, and a definitive diagnosis. This could range from benign findings to adenocarcinoma. A specialist pathologist will detail how many cores show abnormal cells and any presence of margins or perineural invasion.
Understanding pathology language can be challenging. It involves recognizing short phrases that describe cell patterns, inflammation, and specific features critical for prognosis. Lab comments might suggest additional staining or genetic tests for borderline or unusual results.
Gleason scoring is key in grading prostate cancer. The report combines the two most prevalent patterns in the tumor, summing them for a score between 6 and 10. This score is then mapped onto Grade Groups from 1 to 5 for clearer clinical use.
In simple terms, lower Gleason scores indicate slow-growing cancer. Higher scores suggest a more aggressive tumor with a quicker spread. Grade Groups facilitate discussions about risks and outcomes between doctors and patients.
After reviewing the pathology, clinicians determine the next steps. For positive results, staging may involve multiparametric MRI, CT scans, or bone scans based on PSA levels and grade.
A negative biopsy with ongoing concerns often leads to repeat testing. Subsequent procedures might use MRI-guided or transperineal approaches to sample missed areas.
Treatment options vary widely, from active surveillance to radical prostatectomy, radiation therapy, and systemic treatments for advanced disease. The choice depends on cancer grade, PSA, patient age, overall health, and personal priorities.
Shared decision-making is essential. Urologists, radiation oncologists, and medical oncologists often collaborate. A multidisciplinary review ensures the chosen treatment aligns with the patient’s risk profile and lifestyle goals.
| Report Element | What It Means | Common Follow-Up |
|---|---|---|
| Diagnosis (benign vs. adenocarcinoma) | Confirms presence or absence of cancer cells | Negative: monitor PSA; Positive: staging and consult |
| Gleason Score / Grade Group | Measures tumor aggressiveness; guides prognosis | Low grade: consider surveillance; High grade: consider definitive therapy |
| Extent (number of positive cores) | Shows how much tissue is involved | More cores positive may prompt imaging and treatment planning |
| Margins & Perineural Invasion | Suggests local spread patterns | May influence surgical approach or adjuvant therapy |
| Recommendations (additional tests) | Flags need for MRI, genomic testing, or repeat biopsy | Follow tests to refine staging and personalize care |
What To Expect After A Prostate Biopsy And Recovery Tips
Recovery from a prostate biopsy is typically short. Men often experience soreness for a day or two. They can usually return to light activities within 24–48 hours. This section provides practical guidance on what to expect and offers essential recovery tips.
Typical Recovery And Everyday Changes
Men can expect mild soreness in the rectum or pelvis. Blood in urine, stool, or semen is common for days to weeks. Rust-colored semen may last several weeks without posing a risk. These symptoms are usually temporary and do not require emergency care.
Activity, Medications, And Diet
For 24–48 hours, keep activities light. Avoid heavy lifting and intense exercise until the discomfort subsides. Adhere to the prescribed antibiotics to minimize infection risk. Drinking water and using a stool softener can ease bowel movements and reduce strain.
Post-Biopsy Warning Signs That Need Attention
Be aware of warning signs that require immediate doctor’s attention. Seek care for fever or chills, heavy or prolonged bleeding, severe pain, or trouble urinating. These symptoms may indicate infection, significant bleeding, or urinary retention, requiring urgent treatment.
Practical Home Care Tips
- Finish the full course of antibiotics to prevent infection.
- Use over-the-counter pain relievers such as acetaminophen for soreness unless your doctor advised against them.
- Stay hydrated and avoid alcohol for 24–48 hours to reduce bleeding risk.
- Follow any medication‑hold instructions given before the biopsy to minimize bleeding concerns.
When To Seek Urgent Help
If you cannot urinate, develop a fever above 100.4°F, have heavy bleeding, or feel rapidly worsening pain, seek immediate medical attention. Quick action can prevent complications and expedite recovery.
Final Practical Notes
Most men recover fully with rest, fluids, and simple measures. Keep a symptom log for the first week and report any unusual symptoms to your provider. These tips and notes help patients feel prepared and safe during their recovery.
Conclusion
A prostate biopsy is the definitive method for diagnosing prostate cancer, weighing its benefits against risks. It offers tissue sampling for grading and staging, which blood tests and scans cannot provide. This makes it the cornerstone for deciding between treatment and surveillance. Yet, it comes with downsides like bleeding, infection, false negatives, and overdiagnosis.
Recent advancements in technology, such as multiparametric MRI and MRI-targeted fusion biopsies, are changing the game. These innovations improve disease detection and reduce complications associated with older methods. This evolution highlights the dynamic nature of prostate biopsy, not a static verdict.
Decisions on treatment should be tailored to each individual. Factors like PSA trends, MRI results, Gleason scores, patient age, and personal goals are all critical. Consulting with a urologist and sometimes a multidisciplinary team ensures care is aligned with patient values.
In essence, prostate biopsy is a complex tool with both strengths and limitations. When used judiciously, alongside modern imaging and patient-centered discussions, it remains vital for delivering appropriate care to those who need it most.
FAQ
What Is A Prostate Biopsy And Why Is It Done?
A prostate biopsy removes tiny tissue samples using a spring-loaded needle. This is done to check for cancer cells. It’s recommended when PSA levels are high or a digital rectal exam shows abnormalities. The tissue analysis provides a definitive diagnosis and helps determine the best treatment, from active surveillance to surgery or radiation.
How Should Patients Prepare For A Prostate Biopsy?
Urologists ask for a urine sample to check for infections. They also advise stopping blood-thinning medications a few days before. A cleansing enema might be suggested. Prophylactic antibiotics are given to lower infection risk. If an active urinary infection is found, the biopsy is postponed until it’s treated.
What Happens During A Transrectal Ultrasound (TRUS) Biopsy?
During a TRUS biopsy, the patient lies on their side. An ultrasound probe is inserted into the rectum, and local anesthetic is applied. A spring-loaded biopsy gun takes about 10–12 systematic cores from different prostate zones. Each core causes a brief sting. The whole visit and sampling take roughly 20 minutes.
How Is A Transperineal Biopsy Different And When Is It Used?
A transperineal biopsy accesses the prostate through the perineal skin. It often uses MRI or ultrasound guidance. This method provides better sampling of anterior and transition zones. Many centers favor transperineal approaches for repeat biopsies and to lower rectal-flora-related infection risk.
What Are MRI-Targeted And Fusion Biopsies?
Multiparametric MRI can highlight suspicious prostate lesions. MRI-targeted biopsies—done cognitively, with MRI-ultrasound fusion, or in-bore MRI—direct cores to those lesions. Fusion techniques map MRI findings onto real-time ultrasound, improving detection of clinically significant cancers while potentially reducing unnecessary sampling of benign tissue.
What Are The Most Common Side Effects After A Prostate Biopsy?
Short-term effects include rectal bleeding, blood in urine (hematuria), and blood in semen (hematospermia). These are usually minor and self-limited. Soreness and mild urinary discomfort are common for a day or two. Hematospermia can persist for several weeks but is typically harmless.
How Common Are Serious Complications Like Infection Or Urinary Retention?
Serious events are less common but possible. Biopsies can introduce rectal bacteria into the prostate or bloodstream, causing urinary tract infections or, rarely, sepsis—hence routine prophylactic antibiotics and pre-procedure urine testing. Temporary urinary retention sometimes occurs and may require brief catheterization. Significant complications are reported in roughly 3–7% of patients in some series.
Can A Biopsy Miss Cancer? What Are False-Negative Rates?
Yes. Standard 12-core systematic TRUS sampling is not perfect; sensitivity can be limited and false-negative rates up to about 30% have been reported. Random sampling may miss small, anterior, or poorly sampled lesions. When clinical suspicion persists—rising PSA or atypical findings—repeat biopsy often uses MRI guidance or transperineal templates to improve detection.
What Do Pathology Reports From A Biopsy Include?
A pathology report describes the microscopic appearance of cores, notes diagnoses such as adenocarcinoma or benign changes, and assigns a Gleason score or Grade Group when cancer is found. Gleason scores combine two predominant patterns to give a sum (commonly 6–10); Grade Groups 1–5 map to these scores and clarify aggressiveness and prognosis.
If Cancer Is Found, How Do Biopsy Results Affect Treatment Choices?
Biopsy grading (Gleason/Grade Group), the number and location of positive cores, PSA level, and imaging together determine risk category. Low-grade, low-volume cancers are often managed with active surveillance. Higher-grade or more extensive disease may prompt definitive therapy such as radical prostatectomy or radiation. Multidisciplinary discussion and patient preferences guide the plan.
What Is Overdiagnosis And How Often Does It Happen With Prostate Biopsies?
Overdiagnosis refers to finding indolent tumors that would not cause symptoms or shorten life. Systematic biopsies frequently detect small, clinically insignificant cancers; some studies suggest up to half of cancers found this way may be low-risk. Overdiagnosis can lead to anxiety and overtreatment, which carries risks like incontinence and erectile dysfunction.
Can MRI Replace Biopsy For Diagnosing Prostate Cancer?
No. Multiparametric MRI is a powerful noninvasive tool that improves lesion detection and helps decide who needs a biopsy, but MRI cannot confirm cancer histology. Suspicious MRI lesions require tissue sampling for definitive diagnosis. MRI-first strategies can reduce unnecessary biopsies and focus sampling on likely significant disease.
When Should A Repeat Biopsy Be Considered?
Repeat biopsy is considered with persistently elevated or rising PSA, continued abnormal clinical findings, or prior atypical pathology. Repeat procedures commonly employ MRI targeting or transperineal approaches to improve yield and sample previously under-sampled areas.
How Should Patients Recover After A Biopsy And When Should They Seek Help?
Most patients can resume light activity within 24–48 hours. Expect temporary bleeding and semen discoloration. Follow the prescribed antibiotic course and any medication-hold instructions. Contact a provider immediately for fever or chills, severe or prolonged bleeding, worsening pain, or inability to urinate—these may signal infection, significant hemorrhage, or urinary retention.
What Are The Main Benefits Of Getting A Prostate Biopsy?
The chief benefit is definitive, tissue-based diagnosis: confirming cancer, grading its aggressiveness, and guiding staging and treatment. Biopsy identifies cancers that need timely intervention and helps rule out malignancy when screening tests are abnormal. Modern strategies—MRI guidance and transperineal approaches—aim to increase detection of clinically significant cancers while reducing complications and unnecessary treatment.