Focal Therapy for Prostate Cancer: A Modern Approach
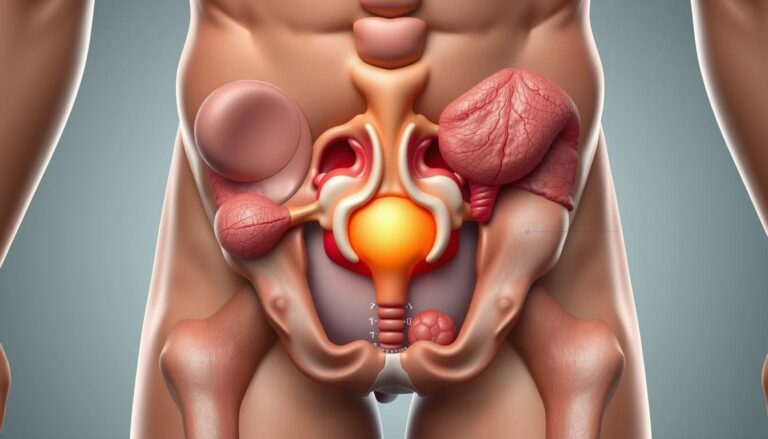
Focal therapy for prostate cancer is a modern approach that spares more tissue than traditional treatments. It targets the tumor or the area around it, aiming to preserve critical structures. This method can significantly reduce the risk of erectile dysfunction and urinary incontinence, common side effects of radical prostatectomy or whole-gland radiation.
This minimally invasive treatment employs various technologies, including high-intensity focused ultrasound (HIFU), cryotherapy, and irreversible electroporation (NanoKnife). Photodynamic therapy and focal brachytherapy are also part of this arsenal. The goal is to balance cancer control with preserving function, using techniques like lesion-targeted ablation or subtotal patterns.
Initial studies show promising results, with high rates of continence and potency compared to traditional treatments. Yet, more data is needed to fully understand the long-term effects. The challenges include accurately localizing significant disease and establishing consistent outcome measures.
Focal therapy offers a targeted approach to prostate cancer treatment, focusing on quality of life while ensuring oncologic safety. Its role is expanding as imaging, biopsy mapping, and trial data improve. This evolution is key to making more personalized decisions in prostate cancer care.
What Is Focal Therapy For Prostate Cancer
Focal therapy is a middle ground between watchful waiting and radical treatment. It targets early-stage disease, aiming to remove or destroy only the tumor while preserving the gland. This method aims to maintain urinary and sexual function, reducing side effects seen with whole-gland treatments.
The core of focal care is patient-centered goals. Men diagnosed through PSA screening often face low- to intermediate-risk cancers. Focal therapy offers benefits like shorter recovery times, fewer hospital days, and lower risk of complications compared to radical prostatectomy or whole-gland radiation. It focuses on preserving quality of life, including continence, potency, and bowel function, while controlling cancer.
The shift from focusing solely on survival to improving life after treatment has sparked interest in targeted prostate cancer treatments. Focal therapy aligns with this goal, aiming for a balance between cancer control and preserving function. It is ideal for men who value maintaining a high quality of life post-treatment.
The index lesion hypothesis guides treatment strategies. Studies indicate that a dominant tumor focus often drives cancer progression. Treating this focus can offer significant benefits while sparing small, low-risk lesions. Patients with larger, visible lesions on imaging are typically the best candidates for focal therapy.
Treatment methods vary from lesion-targeted ablation to region-targeted plans like hemi-ablation. Lesion-targeted treatment focuses on the identified tumor, minimizing collateral damage. Region-targeted treatment, on the other hand, covers a larger area to ensure cancer control. This approach, while potentially more effective, increases the risk of functional compromise.
It’s estimated that half to two-thirds of men with localized disease could benefit from focal therapy. Eligibility depends on tumor distribution, imaging quality, and biopsy results. This makes focal therapy a significant option in localized prostate cancer treatment, embodying targeted treatment in urology practice.
Comparing Prostate Cancer Treatment Options And Where Focal Therapy Fits
Choosing a prostate cancer treatment is like navigating a complex map with multiple paths. Each route offers different trade-offs between controlling the disease and maintaining daily life functions. Focal therapy aims to treat the main tumor while preserving urinary and sexual functions, sitting between conservative monitoring and full removal or radiation.
Radical prostatectomy and definitive radiotherapy aim for a cure. They reduce the risk of cancer spreading but increase the risk of erectile dysfunction, urinary leakage, and bowel irritation. The impact on function varies by center and technique, but the long-term effects are well-documented.
Active surveillance is a conservative approach, suitable for low-risk patients. It involves regular PSA tests, imaging, and biopsies. This approach can cause anxiety and carries a small risk of missing higher-grade disease due to sampling error.
Focal therapy seeks to find a middle ground. Early studies show good short-term cancer control and urinary function preservation in 90–100% of patients. Many patients maintain potency, making focal therapy an attractive option for those prioritizing function.
Guidelines now recognize focal therapy for intermediate-risk tumors, typically Gleason 3+4 and select 4+3, when the main tumor is dominant. It’s also considered for men leaving active surveillance to reduce treatment burden and avoid radical therapy’s full side effects.
Counseling should include realistic expectations. Long-term data are limited, and retreatments may be needed. Radical prostatectomy or radiotherapy remain options after focal ablation, though prior treatment can complicate later surgery or salvage therapy.
Below is a concise comparison to highlight contrasts that matter when discussing prostate cancer management with patients.
| Approach | Primary Goal | Functional Outcomes | Typical Candidates | Notes |
|---|---|---|---|---|
| Active Surveillance | Delay or avoid treatment | Preserves function unless intervention needed | Low-risk, life expectancy >5 years | Requires frequent PSA, MRI, and biopsies; psychological burden possible |
| Radical Prostatectomy | Curative intent | Higher rates of erectile dysfunction and incontinence | Localized disease, fit for surgery | Robotic or open approaches; oncologic control strong in experienced centers |
| Definitive Radiotherapy | Curative intent | Risk of erectile dysfunction and rectal toxicity | Localized or locally advanced disease; nonsurgical candidates | Includes external beam and brachytherapy options |
| Focal Therapy | Target dominant lesion, preserve function | High continence rates; many retain potency | Unifocal/unilateral or index-lesion–dominant disease; select intermediate risk | Considered a prostate cancer surgery alternative; may require retreatment; limited long-term data |
Patient Selection Criteria For Focal Therapy
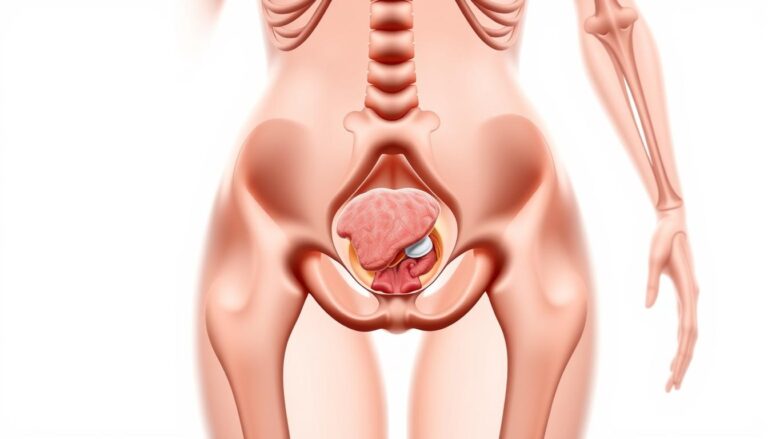
Deciding who benefits from focal therapy for prostate cancer requires a blend of scientific analysis and patient preferences. A thorough screening process identifies men whose disease, anatomy, and life goals align with a targeted treatment approach. The foundation of this selection process is based on detailed imaging and biopsy results.
Imaging And Biopsy Prerequisites
Multiparametric MRI (mpMRI) is a cornerstone in modern prostate cancer management. It helps detect significant lesions and guides biopsies. International guidelines recommend using mpMRI, followed by MRI-targeted plus systematic biopsy for most candidates.
Transperineal template prostate mapping (TPM) biopsy offers detailed three-dimensional mapping, with a sensitivity near 95% for significant cancer. This method requires general anesthesia and carries a small risk of urinary retention. MRI-TRUS fusion biopsy is a less invasive alternative. If mpMRI is not accessible, 3D mapping biopsies are advised.
Clinical And Pathological Factors
Ideal candidates have tumors that are clinically localized (≤T2c), visible on mpMRI, and often unifocal or unilateral. Many centers prefer intermediate-risk disease—Gleason 3+4—though some low-risk men on active surveillance may opt for focal treatment. PSA levels are usually under 10 ng/mL, but some programs consider values up to 20 ng/mL cautiously.
Prostate size is a critical factor in planning. Volumes below 50 ml are preferred for easier energy delivery. Larger prostates are not absolute exclusions. The choice of ablative technology and technique can accommodate bigger glands. Evidence of extraprostatic extension or seminal vesicle invasion argues against focal therapy unless managed by expert teams.
Patient Considerations And Expectations
A life expectancy of roughly 8–10 years is a common threshold for focal intervention. Men should understand that baseline erectile dysfunction does not automatically preclude treatment. Mild to moderate lower urinary tract symptoms require honest counseling and tailored procedural planning.
Patients must accept close surveillance after treatment, the possibility of retreatment, and current limits in randomized long-term data. Salvage focal therapy after radiotherapy is emerging. Shared decision-making, guided by clear imaging and biopsy results, remains essential to smart patient selection focal therapy choices.
Imaging, Mapping And Localization Techniques
Accurate localization is key to precise focal therapy. Imaging and systematic biopsy work together to map cancer within the gland. This guides treatment planning and reduces the chance of missed disease. A pragmatic pathway blends high-quality scans with targeted and mapping biopsies to create a three-dimensional view clinicians trust.
Multiparametric MRI And Reporting Standards
Multiparametric MRI prostate combines T2-weighted anatomy with diffusion-weighted imaging and dynamic contrast sequences. These elements boost lesion detection and help characterize volume and location. Sensitivity is often reported between 86–95% for lesions larger than 0.5 ml.
Reporting follows standardized systems such as PI-RADS to improve consistency between centers. Expert uro-radiologists enhance reproducibility, reduce false positives, and make focal therapy imaging more actionable for urologists and radiation oncologists.
Biopsy Strategies: MRI-Targeted, Systematic, And TPM
MRI-targeted biopsy, whether via MRI-TRUS fusion or in-bore sampling, raises detection of clinically significant tumors. Randomized data from trials like PRECISION support the value of mpMRI before biopsy, then targeting suspicious lesions.
Systematic sampling remains essential to survey areas that appear negative on imaging. Many teams favor the transperineal approach because it lowers infection risk compared with transrectal routes and suits mapping protocols.
Transperineal template mapping (TPM) at roughly 5 mm intervals gives three-dimensional coordinates and near-complete coverage. TPM sensitivity for clinically significant lesions approaches 95%, making it the recommended standard for thorough biopsy mapping prostate when definitive localization is required.
Emerging And Adjunctive Imaging
PSMA PET is becoming a useful adjunct for nodal and distant staging and may find a routine spot in focal therapy workflows as evidence grows. It helps detect occult disease that conventional imaging can miss.
Contrast-enhanced ultrasound, elastography, and advanced tissue characterization tools provide extra information at some centers. Their roles remain adjunctive, supporting decision-making but not replacing core multiparametric MRI prostate or TPM when selecting candidates.
| Modality | Primary Role | Strengths | Limitations |
|---|---|---|---|
| Multiparametric MRI prostate | Lesion detection and characterization | High sensitivity for index lesions; anatomical and functional detail; PI-RADS framework | Operator-dependent; limited for very small lesions; requires uro-radiology expertise |
| MRI-Targeted Biopsy (Fusion / In-Bore) | Confirm imaging targets with directed sampling | Improved detection of clinically significant disease; less overdiagnosis of indolent tumors | May miss multifocal disease if not paired with systematic sampling |
| Systematic Transperineal Biopsy | Survey of the entire gland | Lower infection risk; complements targeted cores; adaptable to office or theater settings | Sampling error persists; may require anesthesia for extensive mapping |
| Transperineal Template Mapping (TPM) | Comprehensive biopsy mapping prostate | Three-dimensional coordinates; ~95% sensitivity for significant lesions; gold standard pre-focal assessment | More invasive; resource-intensive; requires specialized equipment and planning |
| PSMA PET | Staging and detection of occult disease | High sensitivity for small nodal or metastatic deposits; refines treatment extent | Cost and availability limit routine use; role in focal therapy is evolving |
| Contrast Ultrasound / Elastography | Adjunct lesion characterization | Real-time imaging; can guide biopsies in some settings | Variable performance; not yet standard for primary selection |
Ablative Technologies Used In Focal Therapy
Focal therapy technologies offer several methods to target and destroy cancerous parts of the prostate. This approach aims to preserve the rest of the prostate. Each method employs different physics and delivery methods, each with its own recovery and function trade-offs. The following sections detail the main options and their roles in clinical practice.
High-Intensity Focused Ultrasound
High-intensity focused ultrasound (HIFU) uses transrectal probes to focus sound waves into a precise area. This creates temperatures above 80 °C, leading to tissue damage and cavitation.
HIFU is most effective in glands under 40 mm in anteroposterior diameter. It’s also beneficial after a cytoreductive step reduces the gland’s size. Its appeal lies in its short recovery time and outpatient treatment.
Studies show high rates of continence and potency among select patients. Biopsy-free rates range from 77% to 92% at six to twelve months. Some residual disease may not be clinically significant. Yet, it faces challenges with anterior tumors and focal zone displacement.
Cryotherapy
Cryotherapy involves inserting argon-based cryoprobes through the perineum to create ice-balls. These ice-balls freeze tissue below −30 °C, causing cell damage and microvascular ischemia.
Tools like urethral warming devices and thermocouples help protect nearby structures. It’s suitable for hemi-ablation and targeted treatments. Yet, planning is critical for tumors near the sphincter to avoid dysfunction.
Continence rates range from 96% to 100%, while potency varies from 71% to 90%. Many recurrences occur in untreated lobes, highlighting the need for thorough mapping before treatment.
Irreversible Electroporation (NanoKnife / IRE) And Other Modalities
Irreversible electroporation (IRE) uses ultra-short electrical pulses to create nanopores in cell membranes. This leads to apoptosis, preserving connective tissue and nerves.
NanoKnife IRE is ideal for lesions near neurovascular bundles or the urethra. It’s also beneficial for larger or irregular glands where tissue preservation is key. Its non-thermal mechanism reduces collateral damage.
Other focal tools include photodynamic therapy, focal brachytherapy, and focal laser ablation. Direct comparisons between these technologies are rare. Clinicians often view them as complementary, not competing.
| Modality | Mechanism | Strengths | Limitations | Reported Functional Outcomes |
|---|---|---|---|---|
| HIFU | Focused ultrasound heating to >80 °C causing coagulative necrosis | Non-invasive, outpatient, rapid recovery; precise focal heating | Challenges with anterior lesions and large glands; edema can shift focal zone | Continence 90–100%, potency 89–95% in select series |
| Cryotherapy | Argon cryoprobes creating ice-balls | Effective for hemi-ablation and targeted lesions; durable cold zone | Risk near sphincter; untreated lobes may harbor recurrence | Continence 96–100%, potency 71–90% in reported series |
| IRE (NanoKnife) | Ultra-short electrical pulses creating nanopores and apoptosis | Spares connective tissue and nerves; good near critical structures | Requires precise electrode placement; limited long-term randomized data | Early reports show favorable preservation of function; data evolving |
| Other Modalities | PDT, focal brachytherapy, focal laser (varied mechanisms) | Alternative tissue effects; options for specific anatomy | Heterogeneous evidence base; technique-dependent outcomes | Functional results vary by modality and center experience |
Guidance And Treatment Delivery: From MRI Fusion To MRI-Guided Ablation
The path from imaging to treatment has transformed how urologists approach prostate care. It involves precise mapping, real-time monitoring, and careful perioperative steps. These elements significantly impact outcomes and patient comfort. The technology used influences workflow, cost, and the doctor’s confidence during treatment.
MRI-TRUS Fusion And Software Registration
Platforms from Philips, Siemens, and GE enable the overlay of mpMRI lesion outlines on live transrectal ultrasound. This fusion enhances the accuracy of targeted biopsies and ablations, surpassing traditional methods.
Software registration plays a key role in reducing uncertainty. It aligns landmarks and deforms the MRI to match the ultrasound frame. This ensures more precise energy delivery during focal therapy.
Intra-Procedural MRI Guidance And Challenges
Performing ablation within an MRI scanner offers real-time visualization of the prostate. Thermal maps and immediate imaging feedback confirm treatment adequacy.
Executing therapy in the scanner necessitates MRI-compatible devices and a trained team. The setup is expensive, and sessions are lengthy. This limits availability at many centers, despite the clear benefits for complex cases.
Perioperative Considerations And Catheterization
HIFU and IRE treatments are often performed as outpatient procedures under regional or general anesthesia. Patients usually return home the same day, with clear instructions on activity and fluid intake.
A temporary urinary catheter is frequently used to manage edema and prevent retention. The duration of catheterization varies by center and intraoperative findings. Thoughtful perioperative planning and early follow-up minimize complications.
Common risks include urinary retention and urinary tract infections. Rare complications, such as urethral strictures or fistulas, have been reported. Preoperative counseling and post-op monitoring are essential for early detection and timely management of these issues.
Outcomes, Complications And Surveillance After Focal Therapy
Focal therapy has emerged as a middle ground between active surveillance and radical treatments. Initial studies highlight the preservation of prostate function while treating cancer. It’s important to consider both short-term benefits and the need for more long-term data when evaluating this treatment.
Functional Outcomes And Quality Of Life
Early studies show high rates of continence after focal therapy. Many patients experience near-complete urinary control. Erectile function varies, influenced by initial condition and treatment type.
Studies on HIFU often report 89–95% potency in specific groups. Cryotherapy series show 71–90% potency, depending on patient selection. These outcomes are key for men considering focal therapy.
Quality-of-life improvements are a major draw for some. The hope of fewer long-term side effects is a significant factor in the decision-making process.
Oncologic Control And Limitations Of Existing Evidence
Biopsy-negative rates post-ablation range from 60–92% across various modalities and centers. Initial results are encouraging in many case series. Yet, randomized trials comparing focal therapy with other treatments are scarce.
Guidelines advise caution in interpreting outcomes and encourage participation in trials. Larger, longer studies are needed to establish long-term control and survival rates.
Common Side Effects And Adverse Events
Common complications include urinary retention, infections, and strictures. Rates vary, with urinary retention reported between 2% and 24%. Rare cases of rectal injury or fistula have been documented.
Major complications are rare in mixed-technology registries, sometimes under 2%. The risk profile changes with the device, operator skill, and patient anatomy. Clear counseling about possible side effects is critical.
Surveillance Strategy After Focal Therapy
Follow-up involves regular PSA tests, MRI, and targeted biopsies. This strategy aims to detect recurrence and progression early.
Retreatment options include repeat focal ablation, radiation, or radical prostatectomy. Salvage focal procedures after primary radiation are emerging. Men should understand that retreatment may be necessary and that surveillance is lifelong.
A brief table below summarizes typical functional and oncologic signals reported across focal techniques to aid comparison.
| Measure | Typical Range | Notes |
|---|---|---|
| Continence Rates | ~95–100% | High in most early series; depends on baseline and procedure |
| Potency Preservation | 71–95% | Varies by HIFU, cryo, IRE and baseline function |
| Biopsy-Negative Rates | 60–92% | Short- to medium-term; heterogenous study designs |
| Major Complications | Operator and device dependent; rare serious events | |
| Common Minor Events | 2–24% | Urinary retention, infection, irritative symptoms, strictures |
Controversies, Research Gaps And Future Directions
Focal therapy stands at a critical juncture, balancing between its promising aspects and the uncertainties surrounding it. The ongoing debates on patient selection, study design, and long-term outcomes are intense. These discussions involve urologists, radiologists, and oncologists, shaping current practices and guiding future research.
Selection Paradigms And Role Of Biomarkers
There is no universally accepted criterion for focal treatment eligibility. Many institutions follow a diagnostic pathway that includes multiparametric MRI and MRI-targeted biopsies. The PSA cutoffs vary, ranging from under 10 ng/mL to up to 20 ng/mL in some cases.
Life expectancy of eight to ten years often determines candidacy. Genomic classifiers from companies like Oncotype DX and Decipher hold promise for refining risk assessments. Yet, biomarkers for prostate cancer are not yet standardized for focal therapy selection. Further validation is essential before these tools can become routine.
Need For Randomized Trials And Standardized Endpoints
The scarcity of high-quality randomized trials comparing focal therapy to other treatments creates uncertainty. This uncertainty pertains to long-term cancer control and survival benefits.
Trials need to define treatment failure and biochemical recurrence clearly. Standardized endpoints for oncologic and functional outcomes are necessary. This will enable comparison and meta-analyses across studies.
Technological Advances And Combination Strategies
Advances in imaging and guidance are transforming the field rapidly. Improved mpMRI, PSMA PET scans, and MRI-TRUS systems enhance lesion detection and targeting. New ablative technologies like irreversible electroporation (NanoKnife) and photodynamic therapy are expanding treatment options.
Combination strategies are gaining popularity. Researchers are exploring focal ablation alongside systemic biomarkers to set margins. They also use two modalities for lesions in challenging locations. Centers are tailoring therapy to tumor anatomy using HIFU, IRE, and MRI-fusion guidance.
- Research priorities include rigorous trials and harmonized outcome measures.
- Adoption of PSMA imaging and transperineal mapping may reduce sampling error.
- Integration of biomarkers prostate cancer with imaging could sharpen selection.
To address prostate cancer research gaps, collaboration across specialties is essential. Trials must reflect real-world practice. Thoughtful design and shared endpoints will help move targeted prostate therapy from pilot studies to reliable care pathways.
Conclusion
Focal therapy for prostate cancer represents a modern, patient-focused approach, bridging the gap between active surveillance and whole-gland treatments. Initial results with HIFU, cryotherapy, and irreversible electroporation are encouraging. They show effective preservation of urinary and sexual functions, alongside satisfactory short-term cancer control in selected patients.
The success of focal therapy hinges on precise imaging and mapping techniques. Multiparametric MRI, targeted biopsy, and template mapping are essential for identifying the right candidates. These methods help in choosing the most appropriate energy modality for each patient, based on their anatomy and treatment goals.
Despite its promise, focal therapy faces challenges. The lack of long-term randomized data and varying selection criteria across centers are significant hurdles. Standardized endpoints and surveillance protocols are also evolving. As imaging, biomarkers, and ablation technologies advance, focal therapy may solidify its role in prostate cancer management. It offers a targeted approach that balances cancer control with preserving quality of life.
FAQ
What Is Focal Therapy For Prostate Cancer?
Focal therapy is a method for treating localized prostate cancer. It aims to destroy the tumor while preserving surrounding tissues. This approach uses advanced imaging and targeted ablation, unlike whole-gland treatments. It aims to reduce side effects common in radical prostatectomy and radiation.
What Are The Main Goals And Rationale Behind Focal Therapy?
The goal of focal therapy is to balance cancer control with preserving quality of life. It falls between active surveillance and radical treatment. This is important in the PSA-screened era, where early detection often leads to overtreatment of low- to intermediate-risk disease.
What Is The Index Lesion Hypothesis And How Does It Guide Treatment?
The index lesion hypothesis suggests a dominant high-grade focus drives cancer progression. Focal therapy may target this lesion or a larger area. Small, low-risk foci are often left untreated, aiming for a balance between cancer control and preserving function.
How Does Focal Therapy Compare With Active Surveillance And Radical Therapies?
Active surveillance avoids immediate treatment side effects but involves repeated testing. Radical treatments aim for cure but have higher side effect rates. Focal therapy offers intermediate control with better short-term outcomes, though long-term data is limited.
Who Is A Good Candidate For Focal Therapy?
Ideal candidates have localized, unifocal disease visible on mpMRI, often with low- to intermediate-risk disease. PSA levels are typically
What Imaging And Biopsy Steps Are Recommended Before Focal Therapy?
International consensus recommends mpMRI followed by targeted biopsy. Transperineal template prostate mapping (TPM) provides detailed lesion mapping. MRI-TRUS fusion biopsy is common, with transperineal approaches preferred to reduce infection risk.
What Ablative Technologies Are Used In Focal Therapy?
Modalities include HIFU, cryotherapy, IRE, photodynamic therapy, and focal brachytherapy. Each has unique strengths. HIFU is noninvasive, while IRE may spare nerves. Randomized trials are lacking, so technology choice depends on tumor location.
How Is Treatment Delivered And Guided During The Procedure?
Treatment uses image fusion for precise targeting. MRI-TRUS fusion platforms overlay MRI contours on ultrasound. Some centers use intra-procedural MRI for direct visualization, though this adds complexity and cost.
What Functional Outcomes And Complications Are Reported After Focal Therapy?
Early studies report high continence rates and substantial erectile function preservation. Common issues include urinary retention and infection. Rare complications like urethral strictures or rectal injury are uncommon in experienced centers.
How Effective Is Focal Therapy For Cancer Control And What Are The Evidence Limits?
Short- and medium-term outcomes vary by modality. Many reports show early control, but long-term data is limited. Patients should be informed about these gaps and the possibility of retreatment.
What Does Post-Treatment Surveillance Look Like After Focal Therapy?
Surveillance includes PSA testing, mpMRI, and targeted biopsies. Retreatment options include focal ablation, radiation, or radical prostatectomy. Close follow-up is essential for targeted control.
Are There Biomarkers Or Tests That Improve Candidate Selection?
Genomic biomarkers show promise but are not yet standard. Current consensus emphasizes mpMRI and targeted biopsy. PSMA PET is emerging as a staging tool.
What Are The Main Research Gaps And Future Directions In Focal Therapy?
Key gaps include randomized trials and standardized definitions. Advances in imaging and technologies will refine therapy. Combination strategies and biomarkers may improve outcomes.