Proton Beam Therapy for Prostate Cancer: Side Effects and Benefits
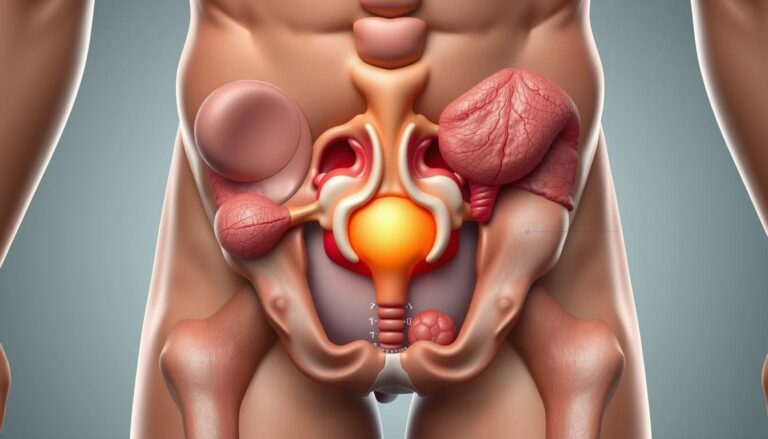
Proton beam therapy for prostate cancer employs charged particles to deliver precise radiation. Unlike traditional X-rays, protons can precisely target tumors, minimizing damage to surrounding tissues like the bladder and rectum.
The goal is straightforward: enhance the therapeutic ratio. This means either increasing cancer control or reducing side effects, such as urinary, bowel, and sexual issues. For many men, this balance is more important than the technical details of treatment.
Curtiland Deville Jr., an associate professor at Johns Hopkins and the medical director of the Johns Hopkins Proton Therapy Center, highlights the advancements in radiation technology. These advancements have led to fewer long-term complications. Studies from other cancer sites suggest shorter hospital stays and a reduced need for feeding tubes, indicating broader benefits of proton therapy.
Despite these advancements, there are practical limitations. Proton therapy is only available at specialized centers, and insurance coverage or cost can significantly influence treatment choices. This article offers a practical, evidence-based look at proton beam therapy for prostate cancer. It aims to assist patients and caregivers in making informed decisions about prostate cancer treatment.
What Is Proton Beam Therapy And How It Differs From Traditional Radiation
Proton beam therapy for prostate cancer employs positively charged particles. These particles release most of their energy at a specific depth, known as the Bragg peak. This results in a sharp drop in dose beyond the tumor. It significantly reduces stray radiation to the rectum and bladder compared to older methods.
Radiation therapy for prostate cancer using x-rays, or photons, scatters dose along its path. Photon beams deliver energy before and after the prostate. This creates a broader dose pattern to surrounding tissues. IMRT, or intensity-modulated radiation therapy, shapes photon dose with multiple beam angles. It aims to spare organs but cannot alter the fundamental physics causing exit dose.
Basics Of Proton Therapy Physics And The Bragg Peak
Protons slow down as they travel through tissue and release their energy at the Bragg peak. Clinicians select beam energy to position that peak within the prostate. Once protons stop, they deliver minimal exit dose. This physics explains why proton therapy side effects may differ from those seen with photon techniques.
Comparison With Photon (X-Ray) External Beam Radiation And IMRT
Photon EBRT sends energy along its entire path, potentially affecting bowel and bladder. IMRT improves shaping, often combined with image-guided radiation to account for motion. Proton therapy, by contrast, changes where the dose ends, not just how it is shaped. This distinction drives clinical debates about trade-offs in cancer control, toxicity, and cost.
How Proton Delivery Techniques (Passive Scatter Vs Pencil Beam Scanning) Affect Dose
Passive scatter systems shape broad proton fields using apertures and compensators. They work well for simple targets. Pencil beam scanning paints the tumor with many small spots. PBS, also called spot scanning, produces finer conformality and reduces dose to nearby structures for complex shapes.
Modern proton centers favor pencil beam scanning for prostate cases because it offers better sparing of healthy tissue. Some clinics use hybrid approaches that mix proton and photon beams when planning calls for tailored solutions. Research continues to compare outcomes and proton therapy side effects across delivery methods.
Understanding Prostate Cancer And When Radiation Is Used
Prostate cancer varies greatly, from small, slow-growing tumors to aggressive forms that spread. Treatment options depend on the cancer’s stage, risk level, the patient’s age, and their life goals. At places like Johns Hopkins Kimmel Cancer Center and Memorial Sloan Kettering, teams of experts from urology, medical oncology, and radiation oncology discuss cases together. This ensures a well-rounded approach to treatment.
Staging is key in determining the cancer’s extent. It distinguishes cancers confined to the prostate from those that have spread. Risk categories—low, intermediate, and high—are based on PSA levels, Gleason scores, and clinical stages. These categories help decide between active surveillance, surgery, or radiation therapy.
Radiation therapy plays a significant role in prostate cancer treatment. It can be used as the primary treatment, alongside hormone therapy for higher-risk patients. This combination aims to improve treatment outcomes.
After surgery, radiation therapy is used to prevent cancer recurrence. This includes adjuvant radiation for positive surgical margins or high-risk pathology. Salvage radiation is an option when PSA levels rise after prostatectomy, aiming to control local disease.
In cases of metastatic disease, radiation therapy has a palliative role. It can target painful bone metastases or control symptoms from bulky pelvic disease. Radiopharmaceuticals like radium-223 or 177Lu-PSMA-617 are used to treat systemic spread, often in conjunction with other systemic therapies.
Proton beam therapy is a type of external beam radiation therapy. It is used in various scenarios, including primary definitive treatment, salvage after surgery, or when sparing tissue is advantageous due to anatomy or prior procedures.
The choice between surgery, IMRT, SBRT, brachytherapy, or proton beam therapy depends on several factors. These include tumor risk, prostate size, prior procedures, baseline urinary and sexual function, and personal preference. Multidisciplinary tumor boards and second opinions help tailor treatment plans to each patient’s needs.
| Clinical Scenario | Common Radiation Options | When Proton Beam Treatment Is Considered |
|---|---|---|
| Low-risk, localized | Active surveillance, EBRT, brachytherapy, SBRT | When organ-sparing or specific dosimetry goals favor protons |
| Intermediate-risk | EBRT ± short-term ADT, SBRT, brachytherapy boost | To reduce dose to rectum and bladder in anatomically challenging cases |
| High-risk, locally advanced | EBRT + long-term ADT, combination with brachytherapy in select cases | When multidisciplinary team prefers proton dosimetry to limit pelvic exposure |
| Post-prostatectomy (adjuvant or salvage) | Post-op EBRT, observation with PSA monitoring | For targeted salvage fields when prior radiation or anatomy raises concern |
| Metastatic/palliative | Palliative EBRT, radiopharmaceuticals | Rarely first-line; considered for symptom control when focused sparing is needed |
Proton Beam Therapy For Prostate Cancer
Proton beam therapy for prostate cancer has evolved from a rare option to a significant part of radiation treatment. Institutions like Mayo Clinic and Johns Hopkins lead in this field, conducting trials to compare it with traditional X-ray treatments. Despite its growing popularity, access remains limited due to the high cost of setting up proton facilities. New, single-room systems are helping to increase availability, but many patients must travel for treatment.
The process starts with a CT scan and sometimes a pelvic MRI to map the prostate and surrounding organs. Teams use specialized tools and techniques to ensure precise targeting. This includes immobilization cushions, bladder and rectal protocols, and fiducial markers or MRI fusion. Small skin marks or tattoos aid in daily setup. Regular imaging and occasional replanning are necessary to maintain dose accuracy as the body changes during treatment.
Treatment schedules for proton beam therapy are similar to external beam radiotherapy. Patients undergo daily sessions, five days a week, for several weeks. Researchers are exploring hypofractionated regimes, which involve fewer sessions with larger doses. Each visit involves positioning and imaging, with beam delivery taking only minutes once the patient is properly set up.
The choice to integrate proton therapy with other treatments depends on the cancer’s risk level. Androgen deprivation therapy is often used alongside radiation for intermediate and high-risk cases. Proton therapy can be the primary treatment, used after surgery for salvage radiation, or combined with brachytherapy for high-risk cases. Multidisciplinary tumor boards make these decisions based on pathology, PSA trends, and imaging.
Success rates of proton therapy are closely monitored in trials and registries. This helps patients and doctors understand its value compared to other treatments. Ongoing research aims to identify which patients benefit most from proton therapy, balancing cancer control with side-effect reduction. Practical considerations such as travel, insurance, and local expertise also influence a patient’s decision to pursue proton beam treatment.
Potential Benefits Of Proton Therapy For Prostate Cancer Patients
Proton therapy presents a unique approach to targeting prostate cancer with radiation. It leverages the Bragg peak to focus the dose within the tumor, minimizing exposure to surrounding organs. This method can significantly alter the patient’s experience of prostate cancer treatment.
Reduced Dose To Surrounding Tissues: Bladder, Rectum, And Penile Bulb
Proton beams rapidly deposit energy at the tumor site, potentially reducing incidental doses to the bladder and rectum. Advanced planning techniques, like pencil beam scanning, further enhance this effect. This could help preserve penile function by minimizing radiation to the penile bulb.
Possibility Of Fewer Urinary, Bowel, And Sexual Side Effects
Common side effects of prostate radiation include urinary urgency, bowel irritation, and erectile dysfunction. By reducing radiation to nearby tissues, these issues might occur less frequently. Initial studies and dosimetric analyses suggest a decrease in symptom severity for some patients.
Lower Theoretical Risk Of Radiation-Induced Secondary Cancers
For younger patients, the long-term risks of radiation-induced cancers are significant. Proton therapy delivers less radiation to normal tissues compared to traditional photon plans. This could lead to a lower risk of secondary malignancies over time.
Emerging Evidence And Examples From Other Tumor Sites Supporting Side-Effect Reduction
Research on esophageal and head and neck cancers indicates fewer hospitalizations and less need for feeding tubes with proton therapy. These findings suggest that reducing normal tissue exposure can yield tangible benefits. Applying these insights to prostate cancer treatment requires direct comparisons.
Comparative studies between proton therapy and modern photon techniques are scarce. The field relies on dosimetry, registries, and retrospective analyses for guidance. The debate continues over the balance between proton therapy’s benefits and its side effects.
Common Short-Term Side Effects After Proton Therapy
Proton beam treatment for prostate cancer brings relief and worry. Short-term effects are common and usually manageable. They often fade after treatment ends. Clinics like the Mayo Clinic and MD Anderson offer close monitoring and clear plans for symptom control.
Fatigue And Recovery Timeline
Fatigue often appears partway through radiation therapy for prostate cancer. It can last weeks to months afterward. Energy tends to return slowly, with many patients reporting steady improvement over three to twelve weeks.
Pacing daily tasks, light exercise like walking, and checking for anemia or mood changes help speed recovery.
Skin Irritation And Localized Soreness
Skin in the treatment field may redden or feel sore, much like a mild sunburn. Symptoms are usually limited to the targeted area. They respond to simple care: gentle cleansing, fragrance-free moisturizers, and loose clothing.
Hair thinning can occur but stays restricted to the treated patch.
Acute Urinary Symptoms And Management Strategies
Radiation can irritate the bladder and urethra, producing urgency, frequency, burning during urination, or occasional blood in the urine. Most men see these symptoms ease after a few weeks. Hydration, urinary analgesics, and alpha-blockers reduce discomfort.
Urologists often adjust medications when prior surgeries like TURP raise risk.
| Symptom | Typical Onset | Usual Duration | Common Management |
|---|---|---|---|
| Fatigue | Midway through course | Weeks to months | Rest pacing, light exercise, check bloodwork |
| Skin Redness/Soreness | Early to mid-treatment | Days to weeks | Topical emollients, mild soap, loose clothing |
| Urinary Frequency/Urgency | During treatment | Weeks after completion | Hydration, analgesics, alpha-blockers, urology follow-up |
| Hematuria (Occasional) | During or shortly after | Short-term, unless severe | Evaluation by urology, urine tests, symptom control |
Possible Long-Term Side Effects And Functional Outcomes
Late effects from prostate cancer radiation can appear months or years post-treatment. It’s vital for patients and healthcare providers to monitor urinary, bowel, sexual, and rare complications. This helps assess long-term quality of life. Proton therapy side effects are part of this broader spectrum, with theoretical dosimetric benefits that may influence long-term outcomes.
Chronic Urinary Issues Including Incontinence And Urethral Stricture Risk
Men may experience persistent urgency, frequency, or leakage long after treatment. Incontinence rates are generally lower than after radical prostatectomy but can increase over time.
Urethral strictures, though less common, pose a significant issue. They can narrow urine flow, leading to slow stream, infections, or bladder problems. Treatment options range from dilation and urethrotomy to urethroplasty when necessary.
Bowel Problems Such As Radiation Proctitis And Management Options
Radiation proctitis can cause rectal bleeding, pain, or urgency. Symptoms may be intermittent and develop long after treatment ends.
Management starts with dietary changes and topical sucralfate or steroid creams. For persistent bleeding, argon plasma coagulation is often used. Specialists in gastroenterology and radiation oncology work together to manage care.
Erectile Dysfunction Risk Over Time And Rehabilitation Approaches
Erectile dysfunction after prostate radiation typically develops gradually. Long-term rates can be similar to those seen after surgery in many studies. Younger men and those with strong baseline function tend to have better outcomes.
Treatment options include sildenafil and tadalafil, vacuum erection devices, intracavernosal injections, and referrals to urology or sexual medicine clinics for personalized rehab plans. Counseling and partner involvement often enhance adherence and outcomes.
Lymphedema And Rare Complications After Pelvic Radiation
Pelvic nodal irradiation can increase the risk of lymphedema in legs or genitalia. Symptoms include swelling and heaviness. Physical therapy, compression garments, and manual lymphatic drainage help manage symptoms.
Rare but serious complications include fistula formation or severe strictures that resist conservative treatment. These often require multidisciplinary surgical care and long-term follow-up within prostate cancer care programs.
Current long-term data comparing proton therapy side effects with other modalities are limited. Dosimetric advantages suggest a possible reduction in late toxicity. Yet, ongoing studies and registries are needed to clarify how these physics translate into everyday outcomes for patients.
Comparing Outcomes: Proton Therapy Versus Other Prostate Radiation Options
Surgeons and radiation oncologists consider several factors when deciding on treatment options. These include cancer control, side effects, and long-term function. Current studies indicate similar biochemical control between photon techniques and proton beam therapy for prostate cancer. This similarity focuses the debate on subtle differences in toxicity and patient selection, not clear superiority in cure rates.
Evidence On Cancer Control And Cure Rates Compared With IMRT And SBRT
Large cohort studies and pooled analyses generally report comparable cancer control across IMRT, SBRT, and proton approaches for localized disease. Randomized trials directly comparing proton therapy success rates with IMRT or SBRT are rare. The available data suggest equivalence in biochemical relapse–free survival when modern planning and dose constraints are used.
Side-Effect Profiles From Observational Studies And Randomized Trials (Where Available)
Dosimetric studies often show lower low-dose exposure to bladder and rectum with proton delivery. Some observational reports note fewer acute urinary or bowel complaints after proton therapy, yet other series find minimal clinical difference. Differences in follow-up, toxicity scoring, and center experience create a mixed picture.
Limitations Of Current Studies And Ongoing Research Needs
Most comparative work is retrospective or uses historical photon techniques. Older passive-scatter proton data sit beside modern pencil-beam scanning series, which complicates direct comparison. Small sample sizes and selection bias limit certainty about true proton therapy success rates in broad practice.
Prospective randomized trials and head-to-head registries remain essential. Research that standardizes fractionation, image guidance, and patient-reported outcomes will clarify whether reduced normal-tissue dose with proton therapy translates to meaningful gains in quality of life or long-term function.
In clinical practice, the choice among prostate cancer radiation options often hinges on patient age, comorbidities, and priorities. For younger men or those with preexisting bowel or bladder issues, the reduced low-dose bath seen with proton plans can tip the balance, acknowledging trade-offs in access and cost.
Treatment Planning And Techniques To Reduce Side Effects
Effective treatment planning combines advanced technology with small adjustments for significant improvements. In prostate cancer care, teams use imaging, physical barriers, and dose strategies to protect vital areas. This approach is essential, whether a center uses photon IMRT or proton beam treatment.
Image-Guided Radiation, MRI Planning, And IGRT Benefits
MRI fusion enhances the prostate’s outline, allowing for precise beam sculpting. This precision avoids damage to nearby organs. Daily IGRT checks ensure accurate positioning, accounting for prostate movement.
Regular imaging reduces margins around the prostate. This reduction minimizes dose to the rectum and bladder, lowering short-term irritation and long-term complications. Both photon techniques and proton beam treatment benefit from MRI planning and IGRT for precise targeting.
Use Of Spacers (Hydrogel) Between Prostate And Rectum
Hydrogel spacers create a gap between the prostate and rectum. This gap reduces radiation dose to the rectum, lowering the risk of radiation proctitis. The gel is biodegradable and inserted in an outpatient procedure.
Spacers complement proton beams and X-ray plans. When paired with MRI-guided planning and precise delivery, they enhance prostate cancer care by preserving bowel function.
Hypofractionation And Fractionation Choices With Proton Delivery
Fractionation impacts treatment convenience and toxicity. Standard fractionation spreads doses over weeks. Hypofractionation, common in SBRT for photons, uses larger doses in fewer sessions.
Proton centers are exploring moderate and ultrahypofractionated courses. These aim to shorten treatment while maintaining dosimetric benefits. The choice depends on cancer control, patient health, and quality-of-life considerations.
Technique synergy is key to minimizing harm. MRI-based contours, hydrogel spacers, daily IGRT, and advanced proton delivery like pencil beam scanning work together. Adaptive planning and periodic imaging during treatment help manage anatomical changes and focus the dose on the target.
| Planning Element | Primary Benefit | How It Supports Proton Beam Treatment |
|---|---|---|
| MRI Fusion | Improved prostate delineation | Reduces margins, refines proton spot placement |
| IGRT (Daily Imaging) | Accurate daily positioning | Accounts for motion, preserves surrounding tissue |
| Hydrogel Spacer | Lower rectal dose | Creates safe separation compatible with proton dose falloff |
| Pencil Beam Scanning (PBS) | Conformal dose shaping | Targets irregular volumes while sparing organs at risk |
| Hypofractionation | Fewer visits, potentially better radiobiologic outcomes | Explored at proton centers to shorten courses with careful toxicity monitoring |
| Adaptive Planning | Adjusts to anatomical changes | Maintains planned sparing during the treatment course |
Cost, Access, And Insurance Considerations For Proton Beam Treatment
Proton beam treatment offers a unique clinical profile, exciting both patients and clinicians. The availability and cost of this treatment vary widely across the United States. Practical planning is as important as the clinical decision-making process.
The number of specialized centers is growing, but it’s smaller than for conventional radiation. Varian and IBA’s single-room systems have made access easier. Yet, many people must travel for treatment. Major centers like MD Anderson and Memorial Sloan Kettering have established programs. New facilities are opening in secondary markets.
Insurance coverage often requires detailed documentation. Carriers may question proton therapy when photon options like IMRT exist. They ask for pathology, staging, prior treatments, and a clear rationale for proton beam treatment. Working with a hospital’s insurance specialists can speed up the process.
For preauthorization, collect pathology reports, operative notes, PSA trends, and multidisciplinary recommendations. Ask the proton center for a letter of medical necessity and for templates used in successful appeals. Clinical trial enrollment can simplify access and reduce costs.
Cost-benefit decisions are critical for individuals and health systems. Proton therapy benefits include lower rates of urinary and bowel toxicity and possibly fewer secondary cancers. These benefits are more significant for younger patients, those needing re-irradiation, and those with unusual pelvic anatomy.
The upfront cost is higher due to capital expenses and maintenance. Some insurers authorize proton beam treatment selectively, prioritizing cases with a clear expected advantage or when other therapies pose higher cumulative harm.
Patients should seek second opinions and meet with financial counselors at the treating center. Discuss bundled pricing, payment plans, charity funds, and whether a clinical trial can cover therapy costs. A clear written plan from the multidisciplinary team strengthens insurance appeals and clarifies expected proton therapy benefits.
| Factor | Typical Situation | Why It Matters |
|---|---|---|
| Center Availability | Major academic centers + growing single-room sites | Determines travel need, local support, and scheduling speed |
| Insurance Approval | Requires detailed documentation and medical necessity | Affects out-of-pocket cost and timeliness of care |
| Patient Selection | Younger age, prior pelvic RT, complex anatomy | Maximizes long-term proton therapy benefits |
| Cost Profile | Higher capital and per-course cost than photons | Drives payer scrutiny and may influence treatment choice |
| Access Strategies | Second opinions, financial counseling, clinical trials | Improves chances of coverage and reduces patient burden |
What To Expect During And After Proton Therapy Treatment
Proton beam treatment for prostate cancer care is a structured process from simulation to follow-up. It aims for precise targeting with minimal disruption to daily life. Here, we outline the typical steps patients go through, along with practical tips on comfort, timing, and monitoring.
Simulation Day, Marks, And Immobilization
On simulation day, a CT scan with MRI fusion is performed to map the prostate. A custom immobilization setup is created using cushions and molds for consistent positioning. Temporary or permanent marks are placed on the skin for daily setup guidance.
Patients are given bladder and bowel prep instructions to maintain organ position. The process is generally comfortable, with staff ensuring proper alignment before leaving.
Typical Session Length, Frequency, And Course Duration
Treatments occur Monday through Friday for several weeks. Some centers offer shorter, hypofractionated courses, reducing session counts. Each visit includes setup and imaging, lasting about 30–45 minutes.
Beam delivery itself is brief, lasting just a few minutes. Continuous visual and audio monitoring allows for quick treatment cessation if necessary. Acute side effects, such as fatigue or urinary irritation, peak near treatment completion and then diminish over time.
Follow-Up Schedule, Surveillance Imaging, And Symptom Monitoring
After treatment, patients are not radioactive and can resume normal activities as tolerated. Follow-up visits include PSA testing and physical exams, scheduled based on risk level.
Periodic imaging may be ordered for higher-risk cases or if symptoms arise. Teams monitor urinary, bowel, and sexual function regularly. Referrals to specialists occur for persistent issues.
Practical Support And Rehab
Many centers, including major academic hospitals like Memorial Sloan Kettering and Mayo Clinic, offer survivorship programs and rehabilitation services. Pelvic floor therapy, medications, and sexual function rehabilitation help manage long-term effects.
Patients seeking to minimize side effects should inquire about spacer placement, bladder/bowel protocols, and symptom-management clinics in advance.
Conclusion
Proton beam therapy for prostate cancer combines physics-driven advantages with practical trade-offs. It focuses the dose on the prostate, sparing the bladder, rectum, and penile bulb. Studies from other tumor sites show significant reductions in clinically important toxicities.
While evidence for prostate cancer is growing, it’s not yet conclusive against modern photon approaches like IMRT and SBRT. Outcomes vary based on patient selection, center experience, and techniques. MRI planning, image guidance, hydrogel spacers, and pencil beam scanning can refine delivery and potentially improve functional results.
Access, cost, and insurance pose barriers for many seeking proton beam therapy for prostate cancer. Multidisciplinary consultation and careful shared decision-making are essential. They help align individual goals—cancer control, quality of life, or minimizing long-term risks—with the most suitable treatment plan.
The landscape is evolving: more centers, improved delivery, and ongoing trials aim to clarify who benefits most. Clinicians and patients must weigh proton therapy benefits against practical constraints as evidence and technology evolve.
FAQ
What Is Proton Beam Therapy And How Does It Differ From Traditional Radiation?
Proton beam therapy uses positively charged particles (protons) instead of x-rays. This method deposits most of its energy at a specific depth, then stops. This precision can reduce damage to nearby organs like the rectum and bladder compared to traditional radiation.
How Do Passive Scattering And Pencil Beam Scanning Affect Dose Delivery?
Passive scattering uses broad proton beams, which are less precise. Pencil beam scanning, or spot scanning, delivers the dose in small spots for better precision. Modern centers prefer pencil beam scanning for complex targets to minimize damage to surrounding tissues.
When Is Radiation Used For Prostate Cancer?
Radiation is used as primary therapy for localized prostate cancer, aiming for a cure. It’s also used with hormone therapy for higher-risk cases. After surgery, radiation may be used if there’s a risk of recurrence. It’s used palliatively for bone pain from metastases.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin marks, and fiducial markers are used. Planning involves target definition, organ-at-risk constraints, and adaptive replanning if anatomy changes.
What Are Typical Treatment Schedules For Proton Therapy?
Most proton therapy courses are five days a week over several weeks. Some centers explore hypofractionated regimens. Each visit includes setup, imaging, and brief, painless beam delivery.
Can Proton Therapy Be Combined With Hormone Therapy Or Surgery?
Yes. Androgen deprivation therapy is often combined with radiation for intermediate- and high-risk disease. Proton therapy can be used postoperatively or with brachytherapy boost in high-risk cases. Integration depends on pathology and multidisciplinary judgment.
What Prostate Cancer Stages Or Risk Groups Might Receive Proton Therapy?
Proton therapy is considered for all risk groups based on disease stage and multidisciplinary recommendations. It’s often chosen for localized and locally advanced disease. The decision depends on tumor risk, prostate size, prior treatments, and patient preferences.
How Does Proton Therapy Fit Into Multidisciplinary Prostate Cancer Care?
Proton therapy is part of a team-based approach with urology and medical oncology. Decisions are made in multidisciplinary clinics. The team weighs options like surgery, IMRT, SBRT, brachytherapy, or proton therapy based on pathology and patient values.
Are Proton Centers Widely Available In The United States?
Availability is growing but remains limited. Proton therapy requires specialized facilities and significant investment. Many patients must travel to centers, with access varying by region.
What Happens During Simulation And Planning For Proton Therapy?
Patients undergo CT simulation, often fused with MRI for accurate prostate delineation. Immobilization cushions, skin