Radiation Treatment for Prostate Cancer & Its Side Effects
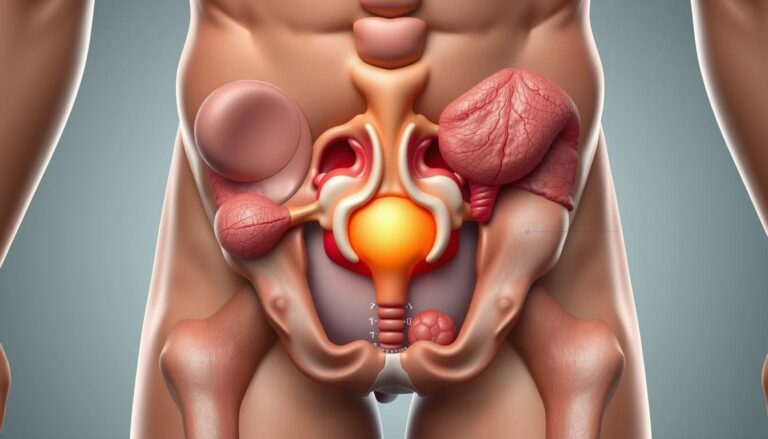
Radiation has become a cornerstone in modern care for men with prostate cancer. Clinicians use high-energy X-rays, photons, protons, or radioactive isotopes to damage tumor cells’ DNA. This stops their uncontrolled growth.
As a primary cure for many early-stage cases, prostate cancer radiation therapy offers outcomes similar to radical prostatectomy for lower-risk disease. It also serves as adjuvant or salvage therapy after surgery. Plus, it acts as palliative treatment to relieve bone pain or control local symptoms when cancer has spread.
Techniques now range from external beam radiation therapy and brachytherapy to radiopharmaceuticals. Advances like IMRT, IGRT, SBRT, MRI-guided linacs, and proton therapy let teams concentrate dose on the gland. This spares nearby bladder and rectum, reducing side effects and shortening treatment time.
Most courses are outpatient and brief each day, though planning and simulation require extra visits. Side effects may appear right away or months to years later. So, follow-up monitoring of PSA and symptoms is essential. Overall, radiation treatment for prostate cancer is versatile and evidence-based. Patients and clinicians weigh effectiveness, side effects, duration, and access together.
What Is Radiation Therapy For Prostate Cancer
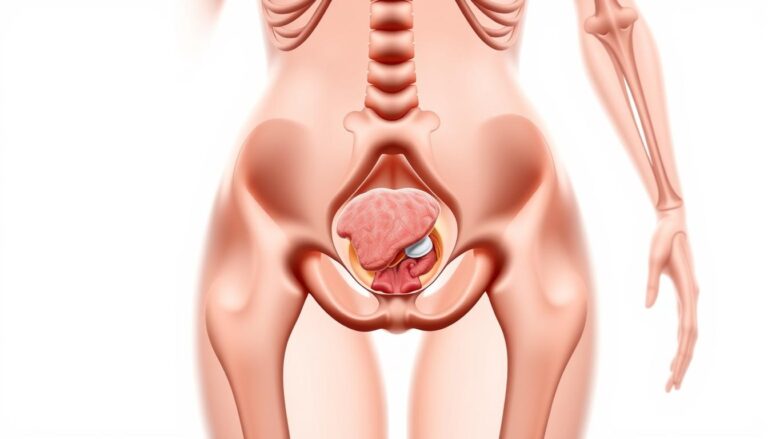
Radiation therapy for prostate cancer targets tumor cells in the prostate gland with focused energy. Radiation oncology teams use imaging and simulation scans to precisely aim beams. Advances like hypofractionation allow for higher doses over fewer visits, protecting nearby organs.
How Radiation Kills Cancer Cells
High-energy beams, such as photons or charged particles like protons, damage cancer cells’ DNA. This damage prevents cell division and triggers cell death over time. Cells that are more sensitive to radiation die sooner, while others struggle to replicate.
The effect of radiation depends on the total dose, dose-per-fraction, and type of radiation. Protons, for example, deposit most energy at a precise depth, sparing tissue beyond the target. The schedule of fractionation affects the balance between tumor control and normal tissue repair.
Goals Of Radiation Oncology For Prostate Cancer
The primary goal is to cure localized disease by eradicating cancer within the prostate. For locally advanced tumors, the focus shifts to durable control and preventing spread to nearby tissues.
Radiation oncology also supports combined strategies. Paired with androgen-deprivation therapy, it targets microscopic disease beyond the gland. After prostatectomy, radiation acts as adjuvant or salvage therapy to reduce recurrence risk when margins or PSA trends indicate concern.
Palliation is another objective. Focused radiation can ease bone pain and other symptoms from metastatic spread, preserving quality of life.
When Radiation Is Recommended
Radiation therapy is often a primary option for low- and intermediate-risk tumors. Patients and clinicians consider tumor features, age, and health when deciding between radiation and surgery.
For higher-risk localized cancer, radiation is commonly paired with androgen-deprivation therapy to improve outcomes. After surgery, rising PSA or adverse pathology may prompt adjuvant or salvage radiation to the prostate bed.
In metastatic settings, radiation provides targeted symptom relief, focusing on painful bone lesions. The final choice depends on stage, risk group, prior treatments, and personal preference.
Radiation Treatment For Prostate Cancer
The choice of radiation is a key part of prostate cancer treatment plans. Options include short, intense treatments and longer, daily sessions. Factors like cancer grade, PSA level, and prostate size are considered. So are urinary symptoms, prior surgeries, and fertility plans.
For cancers stuck in the gland, radiation can be a cure. Techniques like external beam, seed implants, and stereotactic aim to kill cancer cells while protecting nearby organs. Many men with low-risk cancer choose radiation over surgery, with similar outcomes in studies.
Primary Treatment For Localized Prostate Cancer
External beam radiation and brachytherapy are top choices for primary treatment. Seed implants place radioactive seeds in the prostate. Brachytherapy uses temporary catheters for focused doses. Stereotactic body radiation therapy delivers high doses in a few sessions.
Combined Use With Hormone Therapy Or Surgery
For higher-risk tumors, combined treatments are often needed. Androgen-deprivation therapy boosts radiation’s effectiveness. Brachytherapy may be added to external beam for higher doses in some cases.
Radiation is also used after surgery for tumors with risk factors. It treats microscopic disease. For rising PSA after surgery, salvage radiation targets local recurrence.
Palliative Uses For Advanced Or Metastatic Disease
Radiation helps with symptoms from bone metastases and preserves function. A single fraction or short course can quickly ease pain. Stereotactic techniques target specific metastatic spots, sometimes delaying systemic therapy.
Systemic radiopharmaceuticals treat widespread bone disease or PSMA-positive cancer. These agents aim to reduce symptoms and slow disease progression when many sites are involved.
- Schedules vary: SBRT may take days; standard EBRT runs weeks.
- Decision-making blends tumor features with urinary and sexual function goals.
- Teams at centers such as Memorial Sloan Kettering and MD Anderson personalize plans based on risk and patient priorities.
External Beam Radiation Therapy For Prostate Cancer
External beam radiation therapy for prostate cancer employs focused X-rays or particles from outside the body. The process begins with a simulation session, which includes CT scans and often MRI to map the anatomy. Immobilization devices and skin marks ensure each visit is repeatable. The daily treatment time is short, with most of the appointment spent on precise positioning.
The delivery of this therapy relies on a linear accelerator, the machine that shapes and sends beams from multiple angles. During simulation, clinicians place fiducial markers or use pelvic anatomy to guide setup. For EBRT for prostate cancer, imaging before treatment checks prostate position and reduces the risk of missing the target.
How EBRT Is Delivered (Linear Accelerator And Simulation)
Simulation patients lie on a flat table while CT images capture the prostate and nearby organs. Radiation therapists create a plan with dose constraints for bladder and rectum. The linear accelerator delivers each fraction, and therapists monitor the patient on video and with onboard imaging. Reproducible setup keeps doses accurate and side effects lower.
Modern EBRT Techniques: 3D-CRT, IMRT, VMAT, IGRT
Three-dimensional conformal radiation therapy, or 3D-CRT, sculpts beams using CT maps to spare healthy tissue. It set a baseline for safer prostate treatment.
Intensity-modulated radiation therapy, IMRT, adjusts beam intensity across many small segments. IMRT is common for EBRT for prostate cancer because it allows higher tumor doses while protecting the bladder and rectum.
Volumetric modulated arc therapy, VMAT, is a fast version of IMRT. The machine rotates around the patient and often shortens session time. Clinical comparisons show similar tumor control, though studies continue to refine differences in side effects.
Image-guided radiation therapy, IGRT, uses imaging at each fraction to track prostate motion. Daily imaging improves accuracy and can reduce complications tied to misalignment.
Stereotactic Body Radiation Therapy (SBRT) And MRI-Guided Radiation Therapy
SBRT delivers very high doses in five or fewer sessions with tight margins. Systems such as CyberKnife or modern linear accelerators use frequent imaging to lock on the prostate. The major upside is a much shorter overall course of treatment.
Short courses may suit men who prefer fewer visits. Some data suggest certain urinary or bowel effects can be higher in select patients, so candidacy is important.
MRI-guided radiation therapy uses an MRI-linac that shows soft tissues during beam delivery. Real-time tracking lets clinicians pause or gate treatment when the prostate shifts. MRI-guided radiation therapy can sharpen targeting and may spare surrounding structures better than CT-only setups.
Proton Beam Therapy: Pros, Cons, And Availability
Proton beam therapy deposits most energy at a set depth, the Bragg peak, which in theory spares tissue beyond the prostate. That physical property attracts interest for patients with prior pelvic surgery or those seeking dose-sparing to bowel and bladder.
Clinical trials have not proven clear superiority of proton beam therapy for prostate cancer in long-term cancer control. Costs are higher and access is limited because proton centers are fewer in number. Insurance reimbursement can vary by plan and indication.
Choice among conventional fractionation, hypofractionation, IMRT, VMAT, SBRT, MRI-guided radiation therapy, or proton beam therapy depends on tumor risk, anatomy, and patient preference. Precision in targeting and daily imaging remain central to reducing side effects and preserving quality of life.
| Technique | Session Length | Treatment Course | Main Benefit | Common Concern |
|---|---|---|---|---|
| 3D-CRT | 15–30 minutes | 4–8 weeks | Simpler planning, lower cost | Less conformal than IMRT |
| IMRT | 15–30 minutes | 4–8 weeks or moderate hypofractionation | High dose to prostate, spare normal tissue | Longer planning, complex delivery |
| VMAT | 5–15 minutes | 4–8 weeks or hypofractionation | Faster sessions, similar precision | Requires advanced QA and planning |
| SBRT | 20–60 minutes | 1–2 weeks | Very short overall treatment | Higher per-fraction dose risks for some patients |
| MRI-Guided Radiation Therapy | 30–60 minutes | Varies by fractionation | Real-time soft-tissue visualization | Limited availability, longer sessions |
| Proton Beam Therapy | 15–45 minutes | 4–8 weeks or hypofractionation in trials | Potentially less exit dose to tissues | High cost, limited centers, mixed outcome data |
Brachytherapy For Prostate Cancer
Brachytherapy is a precise method for treating prostate tumors by placing radiation sources inside or next to the gland. It is a complementary option to external beam radiation, suitable for men with early-stage disease or as a boost for higher-risk cases. The two main types differ in their timing, dose rate, and patient experience.
Permanent Low-Dose-Rate Seed Implantation
Permanent seed implantation involves placing about 100 tiny radioactive pellets, often iodine-125 or palladium-103, into the prostate. These seeds, roughly the size of a grain of rice, are inserted through needles from the perineum under transrectal ultrasound guidance.
The seeds emit low-dose radiation over weeks to months, remaining in place after their activity diminishes. Some centers use stranded seeds to minimize migration. Patients receive brief advice on radiation precautions, such as avoiding close contact with pregnant women and small children for a short period.
Temporary High-Dose-Rate Brachytherapy
HDR brachytherapy involves placing a high-activity source like iridium-192 into catheters inside the prostate for minutes during each treatment. Courses typically consist of one to four sessions over a couple of days. The catheters are removed after each fraction, ensuring no permanent radioactivity remains.
This method offers steep dose fall-off, sparing nearby tissue while delivering a strong tumor dose. Short-term symptoms may include perineal discomfort and reddish-brown urine for about a week.
When Brachytherapy Is Appropriate And Limitations
Brachytherapy is most effective for early-stage, lower-risk prostate cancer when the gland is a suitable size. It can be used as monotherapy or combined with external beam radiation for higher-risk disease.
Large prostates, prior transurethral resection of the prostate (TURP), and significant urinary symptoms increase the risk of side effects, potentially making the technique unsuitable. Hormone therapy can shrink a large prostate before implantation, making seed implantation for prostate cancer or HDR more feasible.
Preparation And The Implantation Procedure
The procedure is performed in an operating room under spinal or general anesthesia. Imaging with transrectal ultrasound and careful dosimetry planning map seed placement and doses before any needles are inserted.
Patients might stay overnight for observation. For LDR brachytherapy, there is a brief period of radiation precautions and instructions to strain urine in case any seeds are expelled. For HDR brachytherapy, catheters remain in place only during treatment sessions and are removed afterward.
Risks overlap between approaches. Common effects include urinary irritation, frequency, and cystitis. Rare complications include urethral strictures and gradual erectile dysfunction. Rectal irritation or proctitis can occur when nearby tissue receives incidental dose.
Radiopharmaceuticals And PSMA-Targeted Therapy
When prostate cancer spreads, drugs that deliver radiation inside the body become key tools. Radiopharmaceuticals for prostate cancer travel through the bloodstream, attaching to tumor cells or bone metastases. They deliver focused radiation to many sites at once, reaching areas external beams cannot.
How Radiopharmaceuticals Work For Metastatic Prostate Cancer
These agents combine a radioactive isotope with a targeting molecule. The targeting part finds cancer markers or bone turnover, bringing the isotope close enough to damage tumor cells. This local dose can kill cancer cells or shrink lesions while limiting exposure to normal tissues.
177Lu-PSMA-617 (Pluvicto): Indications And Administration
177Lu-PSMA-617 Pluvicto is a PSMA-targeted therapy that binds prostate-specific membrane antigen on prostate cancer cells. It emits beta particles that damage cancer DNA. Clinicians use it for PSMA-positive metastatic castration-resistant prostate cancer after prior hormone therapy. A PSMA PET scan confirms target expression before treatment.
Treatment is given by IV infusion roughly every six weeks, commonly up to six cycles. Blood counts and kidney function are checked before each dose. Reported side effects include fatigue, dry mouth, nausea, appetite loss, constipation and blood count drops such as anemia or thrombocytopenia.
Bone-Targeting Radiopharmaceuticals (Radium-223, Strontium-89, Samarium-153)
Bone-targeting radiopharmaceuticals concentrate in areas of high bone turnover caused by metastases. Radium-223 is an alpha-emitter with survival benefit in symptomatic bone-metastatic castration-resistant prostate cancer. Strontium-89 and samarium-153 are beta-emitters used mainly for pain relief.
Choice among these agents depends on whether disease is limited to bone, presence of visceral metastases, prior therapies and blood counts. Radium-223 suits patients with symptomatic bone disease without significant marrow compromise.
Precautions And Post-Treatment Guidance
Monitoring and simple precautions help reduce risks. Regular complete blood counts and renal tests catch hematologic or kidney effects early. Patients are advised to stay hydrated and void often to lower bladder and kidney exposure.
Because radiopharmaceuticals emit radiation for a short period, patients should limit close contact with young children and pregnant people for the recommended time. Clinical teams provide specific timing based on the isotope and dose.
Radiopharmaceuticals work best within a multidisciplinary plan. Medical oncologists, nuclear medicine physicians and radiation oncologists coordinate to match the agent to disease pattern, prior treatment, symptoms and organ function.
| Agent | Primary Use | Radiation Type | Key Benefits | Notes |
|---|---|---|---|---|
| 177Lu-PSMA-617 (Pluvicto) | PSMA-positive metastatic castration-resistant disease | Beta emitter | Targets PSMA-expressing cells; systemic control | Requires PSMA PET; cycles ~6 weeks; monitor blood and kidneys |
| Radium-223 (Xofigo) | Symptomatic bone-only metastases | Alpha emitter | Pain relief and survival benefit | Best for bone-predominant disease; check marrow function |
| Strontium-89 | Pain palliation from bone metastases | Beta emitter | Effective for diffuse bone pain | Primarily palliative; monitor blood counts |
| Samarium-153 | Pain palliation from bone metastases | Beta emitter | Rapid pain relief in focal lesions | Usually outpatient; watch for hematologic effects |
Common Short-Term And Long-Term Side Effects Of Radiation
Radiation for prostate cancer can ease the fight against tumors while changing daily routines for a time. Side effects range from mild, temporary symptoms to late effects that appear months or years later. Patients often weigh control of the disease against the impacts on bladder, bowel, and sexual health.
Urinary Changes: Frequency, Urgency, Cystitis, Strictures, Incontinence
Irritation of the bladder lining can cause radiation cystitis. This leads to increased frequency, urgency, burning with urination, and sometimes blood in the urine.
Urinary incontinence is less common after radiation than after prostatectomy, yet the risk can rise with time. A rare late issue is urethral stricture, a narrowing that may need dilation or surgery.
Practical steps include timed voiding, pelvic floor exercises, and medications prescribed by a urologist to ease urinary side effects prostate radiation produces.
Bowel Effects: Radiation Proctitis, Diarrhea, Rectal Bleeding, Rectal Leakage
Proximity of the rectum makes radiation proctitis a frequent concern. Symptoms include diarrhea, rectal bleeding, pain, and a sensation of leakage.
Most bowel symptoms improve over weeks to months. A smaller group experiences chronic changes that require endoscopic treatments, topical therapy, or dietary adjustments to manage long-term effects.
Sexual Effects: Erectile Dysfunction And Fertility Impact
Erectile dysfunction after radiation usually develops slowly. Blood vessel and nerve changes take months to affect erections, so function can decline over time.
Fertility may be reduced. Men who want children should consider sperm banking before treatment. Erectile dysfunction after radiation responds to medications like sildenafil, vacuum erection devices, and penile injections in many men.
Fatigue, Skin Reactions, Lymphedema, And Rare Secondary Cancers
Fatigue is common during treatment and can persist for weeks or months. Activity pacing, light exercise, and good sleep help many patients cope.
Skin over beam-entry sites often reddens and feels like a sunburn. If pelvic lymph nodes are treated, lymphedema can cause leg or genital swelling that physical therapy and compression can manage.
Rarely, radiation increases the lifetime risk of a secondary cancer in the treated field. That risk is low compared with the immediate benefit of treating the prostate cancer.
Patients report practical fixes from diet changes to hydration and avoiding bladder irritants. Most symptoms are manageable with a team approach that includes radiation oncologists, urologists, gastroenterologists, and rehabilitation specialists.
| Symptom | Typical Timing | Common Management Options | When To See A Specialist |
|---|---|---|---|
| Urinary frequency, urgency, dysuria | During treatment to months after | Timed voiding, anticholinergics, pelvic floor therapy | Persistent bleeding, severe pain, recurrent infections |
| Radiation proctitis: diarrhea, bleeding | Weeks to months after treatment | Diet changes, topical mesalamine, endoscopic therapy | Chronic bleeding or worsening pain |
| Erectile dysfunction | Gradual onset over months to years | PDE5 inhibitors, vacuum devices, injections, counseling | Loss of function despite first-line therapies |
| Fatigue and skin changes | During treatment and for weeks after | Rest, light exercise, skin care, topical emollients | Severe fatigue limiting daily life or infected skin |
| Urethral strictures and lymphedema | Late effect: months to years later | Surgical dilation, physical therapy, compression garments | Progressive swelling or urinary obstruction |
| Secondary malignancy | Years to decades later | Long-term surveillance and smoking cessation | New lumps, persistent unexplained symptoms |
Managing And Reducing Radiation Side Effects
Radiation can quietly strain the body. Taking practical steps during treatment can greatly improve comfort and recovery. This section will explore planning tools, lifestyle changes, medications, and support options for everyday life during and after therapy.
Treatment Planning To Protect Healthy Tissue
Modern techniques like beam shaping and daily image checks reduce damage to healthy areas. Image-guided radiation therapy (IGRT) allows for real-time adjustments to target the prostate accurately. Methods like IMRT and VMAT help steer the dose away from sensitive areas.
Rectal spacers, whether gel or inflatable, create a gap between the prostate and rectum. Studies show these spacers lower rectal dose and reduce the risk of proctitis. MRI-guided systems further minimize exposure with motion gating.
Diet, Hydration, And Daily Habits
Making small changes to your diet can help manage bowel and bladder symptoms. Many centers recommend avoiding spicy, high-fiber, and gas-producing foods during radiation. Caffeine and alcohol should also be limited to reduce urgency.
Staying hydrated is key. Aim for two liters of fluid per day, as advised by your care team. Regular, small meals and tracking triggers can also help manage treatment days.
Medications And Clinical Interventions
For bowel urgency or diarrhea, medications like psyllium or loperamide can offer relief. Topical sucralfate or steroid enemas may be needed for focal radiation proctitis. Alpha-blockers and antimuscarinics can help with urinary symptoms.
Bleeding or strictures may require antibiotics, endoscopic procedures, or a referral to urology. Reporting symptoms early allows for timely intervention.
Rehabilitation And Sexual Health Support
Pelvic floor physical therapy strengthens muscles that control continence and helps with lymphedema. Sexual health after prostate radiation is a critical part of recovery planning. Options include phosphodiesterase inhibitors, vacuum devices, intracavernosal injections, and penile implants.
Open discussions with a sexual health specialist and partner-focused counseling can improve outcomes. Starting rehabilitation early increases the chance of preserving function.
Practical Tips From Patients And Teams
- Keep a simple symptom diary to share with your care team.
- Try modest dietary adjustments ahead of problem days.
- Ask about spacers for prostate radiation when planning treatment.
- Clarify IGRT scheduling so imaging fits your routine.
- Request early referrals for pelvic therapy or sexual health support.
Proactive measures and clear communication with radiation oncology, urology, and supportive care teams make managing radiation side effects more manageable. Small changes can add up to better days during and after treatment.
Choosing The Right Radiation Treatment Option
Choosing a cancer treatment path is akin to planning a journey with many stops. It’s influenced by patient health, tumor characteristics, and daily life. Discussing radiation treatment options for prostate cancer helps weigh trade-offs and plan practical steps.
Factors That Influence Choice
Tumor stage, PSA level, and Gleason score guide clinical decisions. Life expectancy and urinary function impact quality-of-life choices. Prior procedures like TURP or prostate surgery alter technical options.
Prostate volume is key for brachytherapy seed suitability. Some prefer shorter treatments; others accept longer ones to lower risks. Personal values, like those for treatment duration, are as important as test results.
Comparing Outcomes
For low-risk tumors, radiation and radical prostatectomy have similar cure rates. Side effects differ, with surgery causing early urinary incontinence. Radiation may lead to delayed erectile changes and bowel or urinary irritation.
Higher-risk disease often requires combined treatments. Adding brachytherapy or androgen deprivation therapy to radiation can improve outcomes. Multidisciplinary teams from urology and medical oncology help tailor these approaches.
Access, Cost, And Availability Considerations
Geography and insurance impact real access. Proton therapy, though effective, is limited and costly. Insurers may restrict coverage, affecting travel and out-of-pocket expenses.
Advanced imaging like PSMA scans improve staging and target treatment. Coverage for PSMA PET varies, limiting routine use. Brachytherapy availability also depends on local expertise.
Questions To Ask Your Radiation Oncology Team
- Which radiation modality and fractionation do you recommend for my case and why?
- What short- and long-term side effects should I expect for my situation?
- Will I need hormone therapy, and what is the likely duration?
- Can you use spacers or IGRT to lower rectal dose and reduce bowel risk?
- What follow-up schedule and PSA monitoring will guide future decisions?
- Should I consider sperm banking or other fertility-preserving steps?
- What are likely logistics, travel needs, costs, and insurance limitations?
Effective decision-making combines clear facts with personal priorities. A shared plan, informed by tumor biology, practical access, and patient goals, ensures a purposeful choice.
Conclusion
Radiation therapy for prostate cancer presents a range of options, from external beam radiation to brachytherapy and radiopharmaceuticals. These treatments are effective for both localized and metastatic disease. Advances in technology, such as IMRT and MRI-guided linacs, enhance precision and reduce side effects to nearby organs.
The choice of treatment depends on several factors, including tumor risk and anatomy. Patients must consider the impact on quality of life, as side effects like urinary and bowel issues are common. Open discussions and a clear follow-up plan are essential for making an informed decision.
For those with metastatic disease, targeted agents like 177Lu-PSMA-617 offer new possibilities. These treatments require careful monitoring and selection based on PSMA PET scans. By discussing treatment options and their implications, patients can align their care with their personal goals and lifestyle.
FAQ
What Is Radiation Therapy For Prostate Cancer and How Does It Work?
Radiation therapy employs high-energy rays or particles to damage cancer cell DNA. This makes it impossible for cells to divide and eventually die. The beams are carefully shaped and planned to target the prostate while sparing nearby organs. Techniques include external beam radiation therapy (EBRT) and internal approaches like brachytherapy.
When Is Radiation Recommended Instead Of Surgery?
Radiation is a primary treatment for many men with early-stage prostate cancer. It offers cure rates comparable to surgery for low- and some intermediate-risk cases. It’s also used after surgery to treat rising PSA levels or adverse pathology. For higher-risk localized disease, radiation is often combined with hormone therapy. In advanced disease, radiation treats symptoms or controls specific lesions.
What Are The Main Types Of Radiation Treatment Options?
The main types include external beam radiation therapy (EBRT), brachytherapy, and radiopharmaceuticals. EBRT encompasses 3D-CRT, IMRT/VMAT, and proton therapy. Brachytherapy involves permanent or temporary implants. Radiopharmaceuticals target metastatic disease, including bone-targeting agents and PSMA-targeted agents.
What Side Effects Should Men Expect During And After Radiation?
Short-term effects include urinary irritation, bowel changes, fatigue, and skin irritation. Erectile dysfunction develops gradually over months to years. Late effects may include persistent urinary or bowel problems and a small risk of secondary cancers. Radiopharmaceuticals can cause nausea, dry mouth, and blood-count changes.
How Can Side Effects Be Minimized And Managed?
Modern techniques like IMRT/VMAT reduce dose to healthy tissues. Hypofractionation and SBRT shorten treatment courses. Symptom management includes alpha-blockers, antidiarrheals, and pelvic-floor therapy. Regular follow-up and multidisciplinary care help manage late effects.
What Should Patients Ask Their Radiation Oncology Team Before Treatment?
Patients should ask about recommended modalities and fractionation, hormone therapy, and side effects. They should inquire about follow-up schedules and PSA thresholds. Questions about fertility or social precautions, costs, and insurance implications are also important.
How Do Radiopharmaceuticals Like 177Lu-PSMA-617 Fit Into Care For Metastatic Disease?
PSMA-targeted radiopharmaceuticals like 177Lu-PSMA-617 target cancer cells systemically. They are used for metastatic castration-resistant prostate cancer after prior therapies. A PSMA PET scan confirms target expression before treatment. Monitoring for hematologic and kidney toxicity is essential.
What Practical Differences Should Men Expect Between EBRT, Brachytherapy, SBRT, And Proton Therapy?
EBRT typically takes several weeks with daily visits. SBRT delivers high doses in a few sessions, requiring precision. Brachytherapy implants radioactive sources directly into the prostate. Proton therapy may reduce dose to surrounding tissue but is less available and often more costly.
How Do Doctors Decide Which Radiation Strategy Is Best For An Individual Patient?
Doctors consider tumor stage, PSA, Gleason score/risk group, prostate size, and urinary function. They also consider prior surgeries, life expectancy, and patient priorities. Multidisciplinary discussion and shared decision-making guide the choice of treatment.